New Study Identifies Five Medication Prescribing Cascades that Risk Older Adults' Health

A new study identifies five medication prescribing cascades that may increase health risks for older adults, emphasizing the need for careful medication review in primary care to prevent adverse effects.
Recent research has highlighted the issue of 'prescribing cascades' among older adults, a phenomenon where one medication leads to the prescription of another to address side effects, potentially increasing health risks. An unintentional cascade can occur when symptoms caused by a medication are mistaken for new illnesses, prompting additional prescriptions that may expose patients to further adverse effects.
Researchers from University College Cork in Ireland analyzed prescription data for over half a million community-dwelling seniors aged 65 and above, spanning from 2017 to 2020. Their study, published in The Annals of Family Medicine, used a prescription sequence symmetry analysis within a year to identify nine potential prescribing cascades. The findings revealed that five of these cascades were significant:
- Calcium channel blockers associated with subsequent diuretic prescriptions,
- Alpha-1-receptor blockers linked to vestibular sedative prescriptions,
- SSRIs or SNRIs leading to sleep aid prescriptions,
- Benzodiazepines followed by antipsychotic medication,
- Antipsychotics subsequently resulting in anti-Parkinsonian drugs.
Additionally, three drug pairs showed negative associations, indicating a lower likelihood of sequence from the first to the second medication, including diuretics to overactive bladder medications, benzodiazepines to antidementia drugs, and NSAIDs to antihypertensive medications. Recognizing these patterns is crucial for primary care clinicians to evaluate potential adverse drug reactions when patients exhibit new symptoms. Incorporating awareness of prescribing cascades can help reduce medication-related harm among older adults.
This research underscores the importance of careful medication management and thorough assessment in primary care settings to prevent unnecessary treatments and protect vulnerable populations.
For more details, refer to the original publication: Ann Sinéad Doherty et al., "Prescribing Cascades Among Older Community-Dwelling Adults," The Annals of Family Medicine (2025).
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
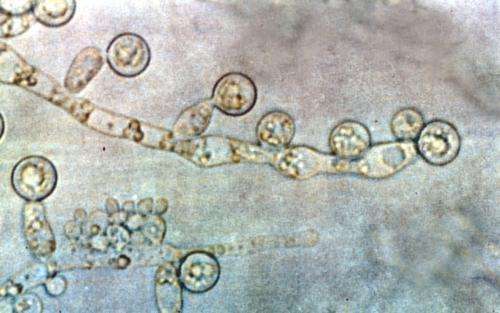
Understanding How Candida albicans Colonizes the Human Gut
New research uncovers the mechanisms behind Candida albicans' ability to colonize the human gut, highlighting potential targets to prevent fungal overgrowth and associated health risks.
Exploring the Connection Between DMT and Near-Death Experiences
Recent studies compare the profound experiences induced by DMT with near-death encounters, highlighting shared features and fundamental differences. Discover how this powerful psychedelic might illuminate the mysteries of consciousness and death.
Metabolism's Role in Breastfeeding’s Protective Effect Against Breast Cancer
Emerging research reveals that a woman’s metabolism, particularly mitochondrial function, influences how breastfeeding can reduce breast cancer risk. Personalized nutritional strategies may enhance protective effects and improve prevention efforts.