AI Set to Influence Medicare Treatment Approvals in Future Policy Trials

The U.S. government is launching a pilot program to test AI algorithms in Medicare treatment approvals, aiming to reduce waste and improve decision-making, but safety and ethics concerns remain.
Starting next year, the U.S. federal government will trial the use of artificial intelligence (AI) to assist in decisions about approving or denying Medicare treatments. Modeled after practices common in private insurance sectors, this pilot program aims to identify potential cost savings by employing AI algorithms to determine the necessity of certain medical services and procedures.
The initiative, called WISeR—an abbreviation for "Wasteful and Inappropriate Service Reduction"—will evaluate whether AI can effectively flag and reduce unnecessary or low-value services such as skin and tissue substitutes, nerve stimulator implants, and knee surgeries. The federal government considers these procedures vulnerable to fraud, waste, or abuse, and believes prior authorization processes, supported by AI, could help mitigate these issues.
The program will operate in select states, including Arizona, Ohio, Oklahoma, New Jersey, Texas, and Washington, starting from January 1, 2026, and will continue through 2031. Notably, certain procedures, like inpatient-only and emergency care, will be exempt from AI assessment to ensure patient safety and timely care.
While AI integration into Medicare has been slow, experts believe this pilot could transform how coverage decisions are made, shifting from traditional contractor-based reviews to AI-assisted ones. Importantly, initial reviews indicate that any AI-driven decision will be reviewed by qualified human clinicians, ensuring oversight and accountability. Vendors participating in the pilot will be incentivized to generate savings without being rewarded for denying legitimate care.
However, concerns are mounting about the potential for AI to reinforce bias, deny necessary care, or be used in a way that prioritizes cost savings over patient health. Critics argue that AI models can be programmed to automatically deny high-cost, high-need services, leading to delays or outright denials that may harm patients, especially those nearing end of life. Transparency and strict oversight are fundamental to addressing these issues.
Policy experts emphasize that ADA algorithms, when properly managed, could reduce delays and administrative burdens. Nonetheless, skeptics warn that the reliance on subjective, sometimes opaque measures, and the possibility of conflicts of interest—such as vendors benefiting financially from less care—pose significant risks. The pilot program remains a cautious step toward implementing AI in healthcare decision-making but highlights the need for rigorous safeguards, transparency, and ongoing monitoring.
The deployment of AI in Medicare is part of broader discussions and debates around leveraging technology for cost control in healthcare. As policymakers and stakeholders evaluate the outcomes of this pilot, the central question remains whether AI can genuinely improve efficiency and patient care without compromising safety and trust.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Rapid Response by Bystanders Can Significantly Increase Survival Rates in Cardiac Arrest Cases
Prompt assistance from bystanders, including CPR and AED use, can significantly improve survival rates in out-of-hospital cardiac arrests, but many lack awareness and training. Learn how quick response efforts save lives.
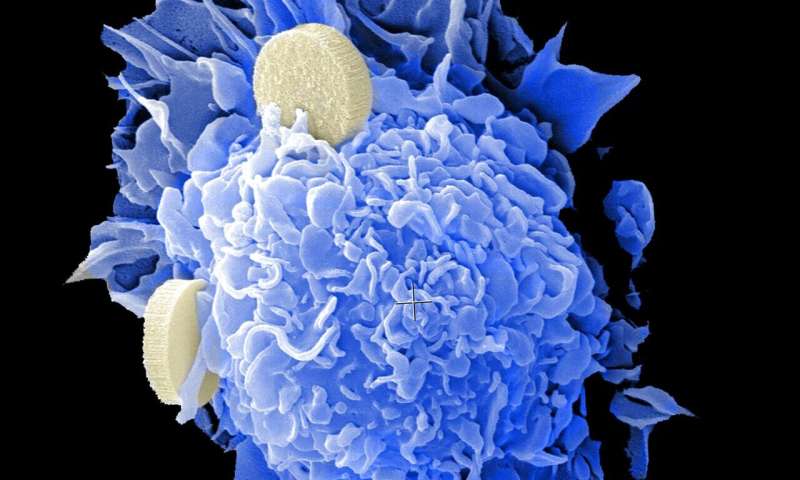
Optimizing a Cancer-Fighting Radioisotope for Targeted Therapy
Scientists at the University of Missouri are advancing cancer treatment with the development of Terbium-161, a versatile radioisotope that offers targeted destruction of cancer cells through enhanced cellular damage mechanisms.
Breakthrough in COVID-19 Recovery: High-Dose Vitamin B3 Targeted at Gut Microbiome Accelerates Healing
A groundbreaking clinical trial demonstrates that targeted high-dose vitamin B3 in the gut accelerates recovery in COVID-19 patients by modulating the microbiome and boosting metabolic processes.
Improved Ventilation in NYC Nail Salons Significantly Reduces Toxic Air Exposure
Research reveals that simple ventilation improvements in NYC nail salons can significantly cut workers' exposure to harmful airborne chemicals, enhancing occupational health and safety.