Primary Care Clinics Effectively Implement Glucose Monitors for Diabetes Management

A study from the University of Colorado demonstrates how primary care clinics can effectively introduce continuous glucose monitors to improve diabetes management, expanding access especially in underserved areas.
A recent study conducted at the University of Colorado Anschutz Medical Campus highlights the promising role of primary care clinics in guiding patients through the use of continuous glucose monitors (CGMs). These small, real-time devices track blood sugar levels, offering a significant advancement over traditional finger-prick tests. The research focused on how primary care practices can incorporate CGMs into routine care, especially in areas lacking access to specialized diabetes care.
Published in BMC Primary Care, the study involved 76 practices in Colorado, which adopted two distinct approaches to initiate CGM use among patients. Some clinics opted for a self-guided method utilizing educational tools designed by the American Academy of Family Physicians, while others referred patients to a virtual CGM initiation service operated by a team of primary care-based health professionals associated with the research project.
Interestingly, practices equipped with in-house diabetes care specialists leaned toward the self-guided route, whereas those without such expertise preferred the remote virtual service. This flexibility demonstrates that clinics can choose the approach best suited to their resources. The core message from the study is that both strategies effectively enabled clinics to start offering CGMs to their patients.
One of the key advantages discussed is the potential for improved accessibility. CGMs help patients better understand how lifestyle factors like food intake, physical activity, stress, and medication influence their blood sugar. This understanding can lead to better glycemic control, fewer complications, and improved quality of life.
Despite the proven benefits, data shows that fewer than half of U.S. primary care physicians have prescribed a CGM. The researchers hope that this study will spur wider adoption of CGMs within primary care, especially in rural areas or regions with limited specialist availability. Using remote support and virtual services, clinics without in-house diabetes experts can offer this life-changing technology.
Dr. Tamara Oser, the senior author, emphasizes that the success of these methods represents a significant step forward in diabetes care. It enables more patients to access modern management tools regardless of their location or the resources of their healthcare provider. This initiative aligns with broader efforts to make diabetes treatment more accessible and effective through primary care, helping more individuals meet their management goals and reduce the burden of diabetes in the U.S.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Promising Results for HER3-Targeted Antibody-Drug Conjugate in Treatment-Resistant Solid Tumors
Early clinical trial results show that the HER3-targeted antibody-drug conjugate DB-1310 offers hope for patients with resistant advanced solid tumors, including EGFR-mutant non-small cell lung cancer, by extending survival and maintaining manageable side effects.
New Immunologic Research Sheds Light on Post-Pandemic Respiratory Virus Resurgence
A recent study reveals how pandemic measures impacted children's immunity, leading to a resurgence of respiratory viruses post-COVID-19 and improving future outbreak predictions.
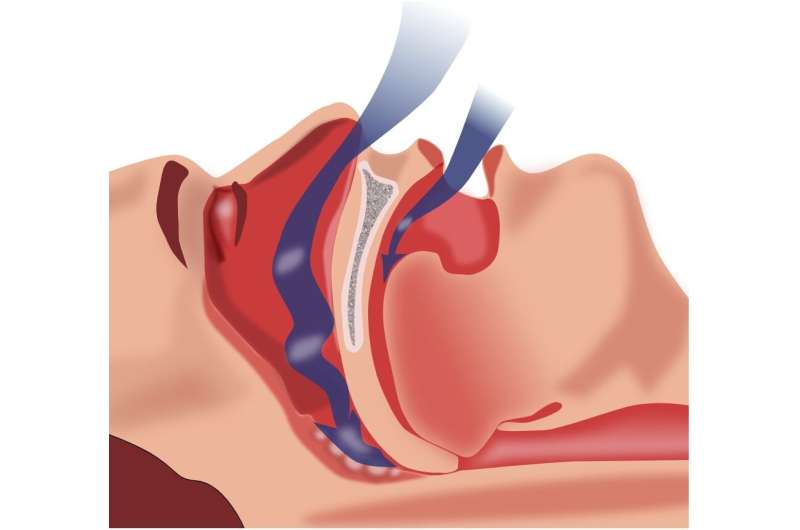
Impact of Obstructive Sleep Apnea on Memory and Brain Health
Obstructive sleep apnea significantly impacts memory and brain function through mechanisms like neuroinflammation and oxidative stress. Early diagnosis and therapy are essential for cognitive health.