Potential Rise in Antibiotic Resistance from Mass Drug Treatments

Research warns that mass antibiotic treatments aimed at reducing child mortality may inadvertently promote the rise and spread of resistant bacterial strains, posing long-term health risks. Ongoing genomic surveillance is crucial.
Recent research led by the University of Liverpool highlights significant concerns regarding the use of mass antibiotic administration (MDA) programs aimed at reducing childhood mortality in regions with high disease burden, particularly in Africa. These programs, which typically distribute antibiotics such as azithromycin (AZM) widely within vulnerable populations, have proven effective in decreasing child deaths. However, new findings suggest that such interventions may inadvertently facilitate the development and spread of antimicrobial resistance (AMR) among bacteria responsible for serious infections like pneumonia and meningitis.
The study, published in The Lancet Infectious Diseases, is a collaborative effort involving UCL, the University of Liverpool, Malawi Liverpool Wellcome Program, the London School of Hygiene & Tropical Medicine, the Wellcome Sanger Institute, and Yale University. It provides the first comprehensive data on how repeated rounds of antibiotic administration influence bacterial populations over time, especially regarding the evolution of resistant strains.
Researchers conducted a comparative analysis of samples from children in areas subjected to multiple rounds of AZM MDA and those in control regions that received a placebo. The focus was on Streptococcus pneumoniae, a common bacterial colonizer of the upper respiratory tract that is responsible for severe illnesses such as pneumonia, meningitis, and sepsis. Through genome sequencing, the team analyzed the bacteria's genetic makeup to identify resistance traits.
Results indicated a concerning increase in resistance to AZM and similar antibiotics, rising from 21.7% to 32.1% three and a half years after the cessation of treatment. Notably, resistance developed not only in treated populations but also appeared to spread into neighboring communities, with resistance levels in placebo regions also rising from 21% to 30.9%. Additionally, some S. pneumoniae strains exhibited resistance to multiple antibiotics including penicillin, which is widely used as a first-line treatment.
Scientific leaders emphasized that resistance to antibiotics like AZM, which was previously thought to diminish once drug use stopped, can persist and disseminate beyond monitored populations. The emergence of multidrug-resistant strains poses a significant challenge to managing bacterial infections, particularly in regions heavily dependent on antibiotics for controlling infectious diseases.
Given these findings, the authors advocate for long-term genomic surveillance to monitor AMR trends in areas employing MDA strategies. This approach could help balance the immediate benefits of reducing child mortality against the potential long-term risks of creating resistant bacterial strains. Dr. Akuzike Kalizang'oma from UCL stressed the importance of carefully weighing these factors, noting that robust monitoring can facilitate timely interventions to prevent resistant strains from spreading extensively.
The World Health Organization (WHO) has supported the use of AZM MDA programs under certain conditions, especially in high-mortality regions. Nonetheless, this new evidence underscores the necessity of ongoing surveillance and judicious antibiotic use. Experts warn that without appropriate intervention, increasing resistance could undermine the effectiveness of antibiotics critical for treating common and life-threatening infections in the future.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
'Barcodes' Written into DNA Uncover How Blood Ages
New research uncovers how DNA methylation barcodes reveal blood cell aging, showing reduced stem cell diversity and clonal expansion linked to age-related inflammation and disease risks.
Discovery of Protein Switch for Regulating Viral and Autoimmune Immune Responses Offers Therapeutic Potential
Scientists have uncovered a vital protein switch involving SLIRP that controls immune responses to viruses and autoimmune diseases, highlighting new therapeutic possibilities for immune regulation.
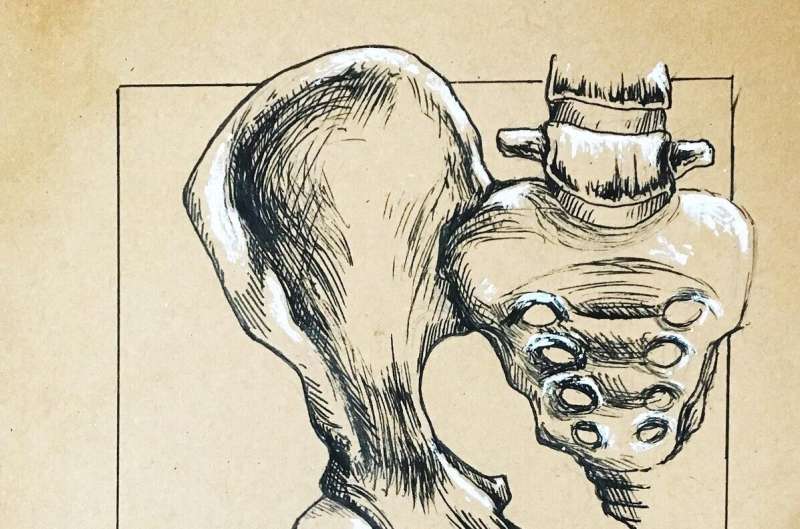
Pelvic Floor Dysfunction: Essential Information for Women
Pelvic floor dysfunction affects up to half of women and can be caused by pregnancy, childbirth, or intense exercise. Learn how to prevent and manage this common condition with effective strategies and exercises.