Innovative Treatment Algorithms Reduce Hospitalizations for Children with Sickle Cell Disease
Implementing standardized treatment algorithms for children with sickle cell disease at MUSC has led to a significant reduction in hospital stays while maintaining patient safety and improving quality of life. Discover how this collaborative approach is shaping future pediatric care.
Recent advancements in the management of sickle cell disease (SCD) have demonstrated that implementing standardized treatment algorithms can significantly improve patient outcomes and reduce hospital stays. At MUSC Shawn Jenkins Children's Hospital, a collaborative effort between the Pediatric Emergency Medicine and Pediatric Hematology/Oncology divisions led to the development of a new protocol specifically for children with SCD presenting to the emergency department with fever, a common and potentially serious complication.
This innovative algorithm involves emergency physicians consulting with hematology and oncology specialists to assess the risk level of each patient. Low-risk children are now eligible for outpatient treatment, as they are deemed unlikely to develop severe complications, thereby decreasing unnecessary hospital admissions. The standardization of care through this protocol ensures consistent decision-making and optimizes patient safety.
Early data collected during the year of implementation revealed a 10% reduction in hospital admissions compared to the previous year, with no increase in readmission rates, indicating that many low-risk patients can be safely managed at home with proper follow-up. The protocol emphasizes predefined risk factors and clear criteria, providing healthcare providers with confidence in their clinical decisions.
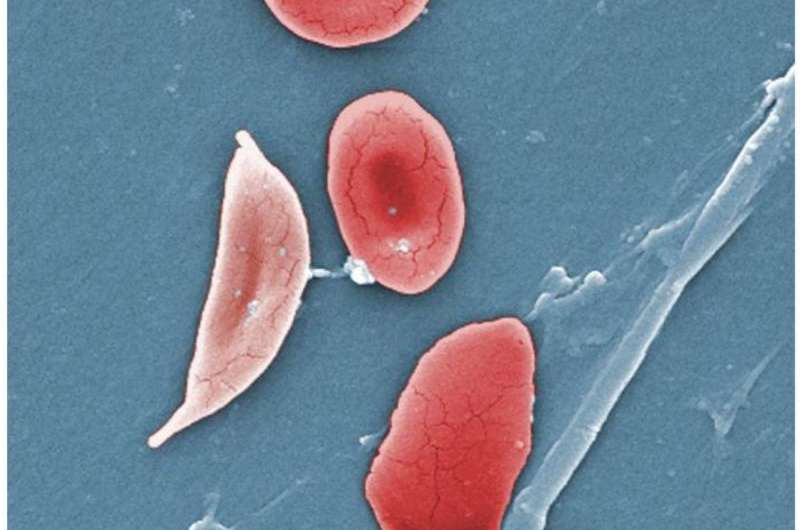
Sickle cell disease is a genetic condition predominantly affecting individuals of African descent. It involves abnormal red blood cells that adopt a sickle shape, impairing blood flow and leading to complications such as chronic pain, respiratory issues, and spleen dysfunction. Monitoring and preventing infections are especially crucial in young children with SCD, due to their increased susceptibility.
The shift to a lowered age threshold for hospital admission from 2 years to 1 year, along with specific criteria, aligns with evolving vaccination protection and national guidelines. Leaders like Dr. Michelle Hudspeth and Dr. Jason Erno emphasize that the algorithm not only enhances safety but also improves quality of life by reducing hospital stays, minimizing disruptions for families, and lowering healthcare costs.
This initiative underscores the value of interdisciplinary collaboration and the potential for protocol-driven approaches to transform pediatric care in chronic disease management. The ongoing use and study of this algorithm at MUSC highlight its success and promise for future broader applications in sickle cell care.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Can Stress Increase Your Risk of Stroke?
Chronic stress significantly increases the risk of stroke by contributing to high blood pressure, inflammation, and unhealthy habits. Learn how stress management can help protect your heart and brain.
Advancements in AI: Deep-Learning Models Mimic Pathologists in Biopsy Analysis
Innovative AI models trained with eye-tracking technology now emulate expert pathologists in analyzing tissue biopsies, promising enhanced accuracy and reduced workload in medical diagnostics.
New Study Brings Hope for Safer Bleeding Treatments
A groundbreaking study from UNC reveals that inhibiting blood clot breakdown may be safer than previously believed, paving the way for improved bleeding treatments without increased risk of harmful clots.
Comprehensive Prehabilitation Strategy Benefits Frail Heart Failure Patients Awaiting Surgery
A multidisciplinary prehabilitation protocol significantly improves physical and cognitive health in frail heart failure patients awaiting surgery, enhancing surgical outcomes and recovery prospects.



