Innovative Approach Reduces Stroke Risk in Heart Failure Patients with LVADs

New research utilizing blood flow modeling offers promising strategies to reduce stroke risk in patients with LVADs, improving the safety and personalization of heart failure treatments.
Left ventricular assist devices (LVADs) are vital for patients with advanced heart failure, significantly enhancing survival and quality of life. These implantable pumps take over the function of the weakened left ventricle, directing blood flow into the aorta and supporting circulation. Despite their benefits, LVADs carry a notable risk: patients face an increased likelihood of developing blood clots that can lead to strokes, with risks ranging from 11% to 47% higher than the general population.
Understanding why some LVAD patients suffer strokes while others do not has been a challenge. However, recent research from the University of Colorado Boulder, CU Anschutz, and the University of Washington has provided new insights by examining blood flow dynamics—called hemodynamics—in these patients. The study involved creating "digital twins" of 12 LVAD patients based on detailed imaging of their vascular structures and clinical data. These virtual models enabled researchers to analyze blood flow patterns before and after LVAD implantation.
The findings revealed significant differences in blood flow patterns among patients who experienced strokes and those who did not. In particular, LVADs can alter blood flow, creating a 'jet' effect that may direct blood into the aorta at unusual angles, potentially promoting areas of stagnation where blood clots could form.
This research highlights the importance of blood flow patterns in stroke risk, offering the possibility of personalized surgical and monitoring strategies for LVAD recipients. By optimizing implant techniques based on hemodynamic data, clinicians may reduce stroke occurrences and improve patient outcomes.
Lead researcher Debanjan Mukherjee emphasizes the role of fluid dynamics in understanding and mitigating risks associated with LVADs, advocating for more research supported by federal funding. Ultimately, these advancements could pave the way for safer implantable heart devices tailored to individual patient profiles.
The broader implications of this work suggest that integrating blood flow analysis into clinical practice may transform how we approach mechanical circulatory support, potentially lowering stroke risks and saving lives.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
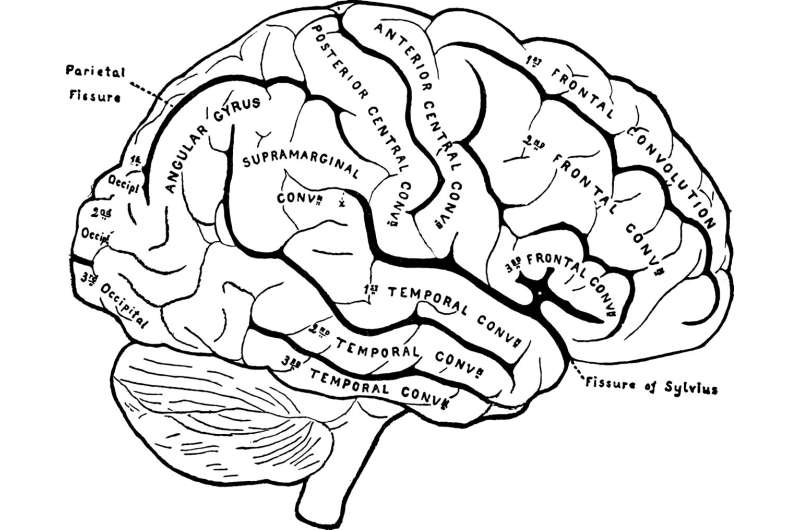
Enhanced Signal Reliability in the Cerebral Cortex Compared to Other Brain Regions
New study reveals that synapses in the cerebral cortex transmit signals more reliably at low calcium levels, highlighting key molecular mechanisms behind brain adaptability and learning.
Impact of Endocannabinoid Receptor Manipulation on Neurodevelopment and Behavior
New research indicates that manipulating endocannabinoid receptors during prenatal development may lead to brain structural changes and behavioral deficits, highlighting potential risks of cannabis exposure during pregnancy.
Understanding the Health Risks for Workers in Engineered Stone Fabrication Shops
New research highlights the health risks faced by workers in engineered stone fabrication shops due to high silica content. Safety measures and regulations are crucial to prevent major respiratory diseases like silicosis.