Growing Concerns as Family Doctors Approach Retirement Age Impacting Primary Care

A new study reveals that many family physicians in Ontario are approaching retirement age, risking primary care shortages. The aging workforce and patient complexity demand strategic solutions to ensure healthcare stability.
A recent study by ICES highlights a significant challenge facing Ontario’s healthcare system: a substantial number of family physicians are nearing retirement age, which threatens the stability of primary care services. Currently, 1.74 million patients are attached to family doctors aged 65 and older, many of whom are elderly with complex medical conditions. This situation raises alarms about an impending shortage of primary care providers as these physicians retire.
The study, published in Canadian Family Physician, examined trends in the composition of Ontario's family medicine workforce—including over 11 million patients and nearly 9,400 comprehensive family physicians as of March 2022. The analysis revealed no growth in the overall number of family physicians, especially among early-career physicians under 35, marking a departure from previous years of workforce expansion.
Interestingly, although many older family physicians continue practicing well into their 70s, their retirement will lead to increased numbers of patients without attached primary care providers. The data also shows that women constitute the majority of the current physician workforce, but the proportion of physicians practicing comprehensive family medicine has declined from 77% in 2008 to 65% in 2022.
Furthermore, a separate study indicated that many family physicians are shifting towards hospital-based work rather than providing comprehensive community care. This trend, combined with the aging workforce, could exacerbate current shortages and impact vulnerable patient populations, including those with chronic conditions like COPD, heart failure, and diabetes.
Experts warn that the primary care system may struggle to accommodate the growing, medically complex patient demographic attached to retiring physicians. Addressing these workforce challenges will require strategic planning, including implementing team-based care models to reduce burnout and support physicians.
Source: https://medicalxpress.com/news/2025-06-family-doctors-nearing-age-future.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Single Dose of Antibiotic as Effective as Multiple Doses for Treating Early Syphilis, Study Finds
A new clinical trial reveals that a single injection of benzathine penicillin G is as effective as multiple doses for treating early syphilis, offering a simpler treatment option and potentially improving patient adherence.
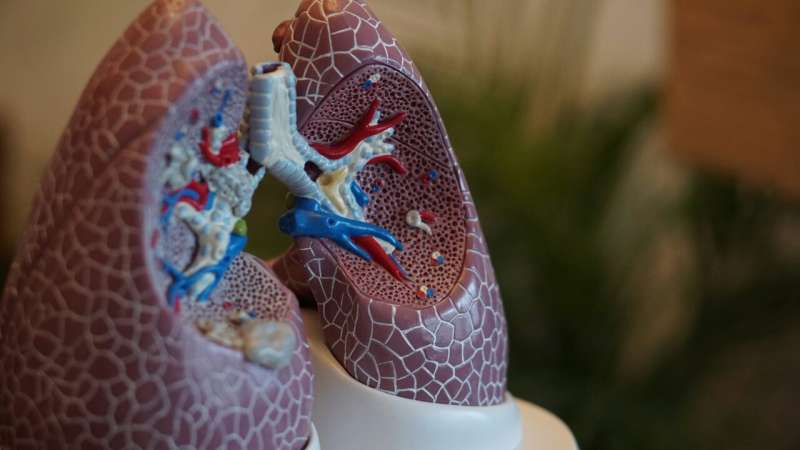
Bronchoscopic Biopsy Techniques as Effective and Safer Alternatives to Percutaneous Methods for Lung Biomarker Testing
New guidelines show that bronchoscopic lung biopsy techniques are as effective as percutaneous methods for biomarker testing while offering greater safety, especially with modern navigational technology.
Innovative Hydrogel Platform Enhances Dendritic Cell Activation for Cancer mRNA Vaccines
A novel hydrogel platform actively recruits dendritic cells to improve the efficiency of mRNA cancer vaccines, promising enhanced immune responses and potential applications in cancer immunotherapy.
The Impact of Degree of Weight Loss on Tirzepatide's Cardiometabolic Benefits
A new study shows that the extent of weight loss during tirzepatide treatment directly impacts improvements in blood pressure, insulin resistance, and cholesterol in adults with obesity or overweight.