Evaluating the Future of Private Health Insurance Rebates and Public Hospital Funding

A comprehensive review of Australia's private health insurance rebates examines their effectiveness in reducing pressure on public hospitals and explores alternative funding approaches for healthcare improvements.
The debate over private health insurance rebates and their impact on public healthcare continues to gain attention in Australia. Currently, around 45% of Australians with private health insurance benefit from government rebates that subsidize their premiums. These rebates—a financial incentive introduced in the late 1990s—aim to encourage private insurance uptake and ease pressure on public hospitals. The government’s expenditure on these rebates is projected to reach A$7.6 billion in 2025, significantly contributing to private hospital funding, which accounts for nearly half of private hospital expenditures.
Private health insurance rebates have historically been part of a broader policy to reduce the burden on public hospitals by incentivizing Australians to seek private care. These rebates are means-tested and indexed annually, with higher subsidies for low-income earners and those over 65. Additional measures accompanying these rebates include Medicare levy surcharges and lifetime health cover loading, further promoting private health coverage.
Despite these policies, evidence suggests that private health insurance may not substantially decrease pressure on the public system. Studies indicate that while individuals with private insurance are more likely to opt for private hospitals, the effect on reducing public hospital wait times is marginal at best. Increasing private coverage does little to alleviate system bottlenecks, and a more effective approach could involve increasing funding directly for public hospitals.
Financial analyses show mixed conclusions regarding the cost-effectiveness of these rebates. A recent study commissioned by Avant Mutual found that the rebates are cost-effective, generating $1.25 in savings for every dollar spent. Conversely, other research indicates that scrapping the rebates could lead to savings exceeding their costs, as it might reduce overall health expenditure. However, these findings depend heavily on assumptions about consumer response to changes in insurance prices.
Responding to these conflicting results, experts highlight that private health insurance does little to significantly impact public hospital wait times. The responsiveness of consumers to insurance prices is low, meaning reductions in rebates may only cause small drops in private insurance membership without drastically affecting public hospital demand.
In light of current cost-of-living pressures, there is an argument for maintaining rebates at their current levels to support household budgets. Still, expanding these rebates appears unjustified given their limited effect on easing public hospital workloads. A more targeted use of funds—such as expanding public healthcare capacity or funding elective procedures in private hospitals—might better serve the overall health system.
Overall, the decision to retain, expand, or remove private health insurance rebates should consider their limited impact on public hospital demand, budget implications, and the potential for more effective allocation of healthcare funding. More independent research is needed to fully assess the long-term costs and benefits of these subsidies.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
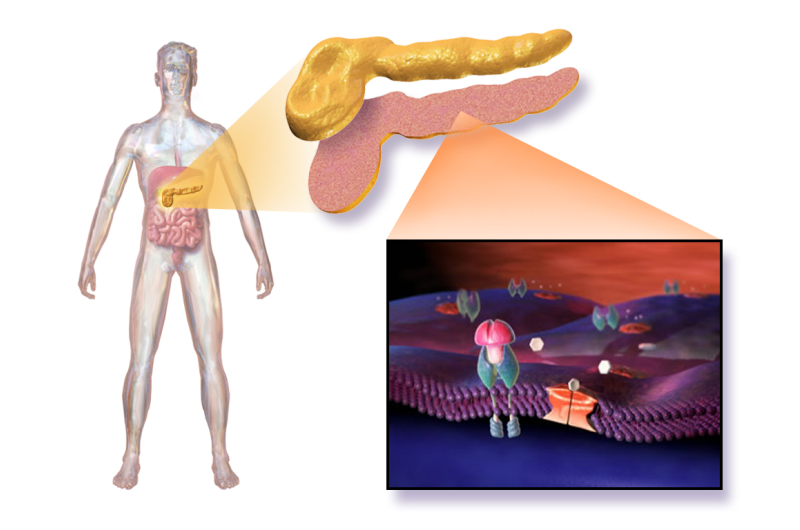
Breakthrough in Gene-Edited Islet Transplant Demonstrates Success in Human Trial
A groundbreaking human trial demonstrates that gene-edited islet cells can survive and function without immune suppression, offering new hope for type 1 diabetes treatment.
Childhood Socioeconomic Disadvantage Associated with Brain Changes in Professional Fighters
A recent study reveals that professional fighters from socioeconomically disadvantaged backgrounds are more likely to experience early brain changes associated with neurodegeneration, highlighting the impact of childhood environment on long-term brain health.
Call for Age-Specific Immunotherapy Approaches in Treating Childhood Brain Tumors
A new review highlights the importance of developing tailor-made immunotherapy strategies to effectively treat childhood brain tumors, considering their unique biology and microenvironment.
Impact of Skin Pigmentation on Pulse Oximeter Accuracy
Recent studies reveal that skin pigmentation can impair pulse oximeter accuracy, especially in low-oxygen conditions, highlighting the need for more inclusive device design. Learn about the latest research addressing this critical issue.