Understanding the Key Differences Between Osteoarthritis and Rheumatoid Arthritis

Arthritis is a common condition that causes pain, swelling, and stiffness in the joints, affecting millions worldwide. Among its many types, osteoarthritis and rheumatoid arthritis are the most prevalent, yet they differ significantly in their causes, symptoms, diagnosis, and treatment. This article explores these differences to help you better understand each condition.
Osteoarthritis is the most common form of arthritis, often seen in older adults. It primarily results from wear and tear of the joint cartilage, which acts as a cushion between bones. Over time, cartilage degeneration leads to joint pain, stiffness, swelling, and sometimes deformity. Commonly affected joints include the knees, hips, fingers, thumbs, and big toes. Risk factors include aging, obesity, previous injuries, and genetics, especially in hand osteoarthritis. Signs can appear around age 45 and tend to worsen with age. However, osteoarthritis is a complex disease affecting the whole joint structure, including cartilage, bones, ligaments, and the joint lining.
Diagnosis usually involves a physical exam and assessment of symptoms. Imaging techniques like X-rays and MRI scans may not always correlate with pain severity, as early-stage damage might not show up yet. There is currently no cure, but symptoms can be managed through exercise, weight management, pain relievers, and anti-inflammatory medications.
Rheumatoid arthritis (RA), on the other hand, is an autoimmune disorder where the immune system mistakenly attacks joint linings, leading to inflammation and joint damage. It often affects smaller joints such as those in the hands and feet but can involve larger joints like knees and elbows. RA typically causes joint pain, swelling, morning stiffness, and can also impact other organs, including the skin, lungs, and heart. It is less common than osteoarthritis, affecting over 500,000 Australians, and can develop at any age, with higher risk between 35 and 64 years. Smoking increases the risk.
Diagnosing RA involves physical examination, blood tests for specific antibodies, and imaging scans like ultrasound or MRI if needed. Early diagnosis is crucial for effective treatment.
Treatment options differ for both conditions. Osteoarthritis management involves lifestyle modifications like exercise and weight loss, along with pain relief options such as topical and oral anti-inflammatories. In some cases, antidepressants are used for pain, but opioids are generally discouraged. Rheumatoid arthritis treatment focuses on preventing joint damage through early use of disease-modifying anti-rheumatic drugs (DMARDs). These drugs suppress the immune response, aiming for remission or symptom control.
Recent advances include research into preventive measures, new medicines to reduce pain, and innovative therapies like immunotherapy for RA that seek to achieve long-term remission. While there is no cure for either type, ongoing research offers hope for better management and potential preventative strategies in the future.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
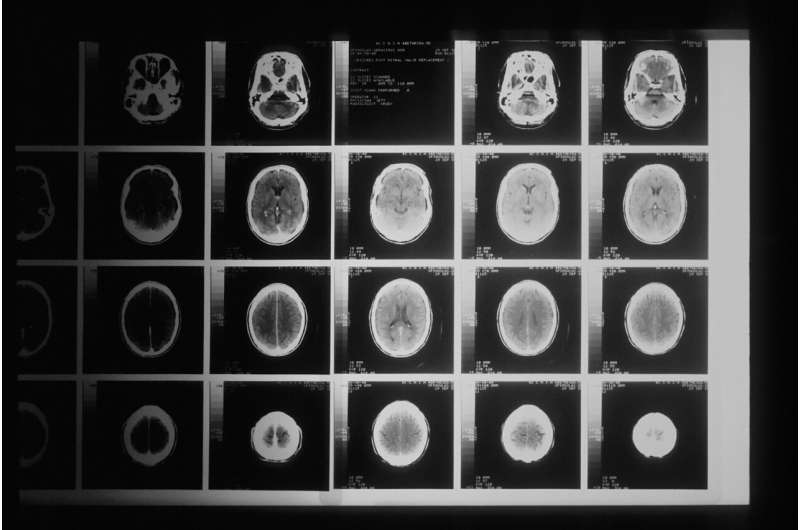
Revolutionary Genetic Test Can Diagnose Brain Tumors in Just Two Hours
A groundbreaking genetic testing method can diagnose brain tumors in as little as two hours, vastly improving intraoperative decision-making and patient outcomes. Developed by the University of Nottingham, this technology uses nanopore sequencing to provide quick, accurate, and cost-effective tumor classification, transforming care for brain cancer patients.
Innovative Genomics Tool Guides Immunotherapy Decisions for Advanced Kidney Cancer
A novel genomics-based tool developed by researchers guides personalized immunotherapy choices for patients with advanced and aggressive kidney cancers, improving treatment outcomes based on tumor immune profiling.