Understanding Mucus Color: Does Yellow Mucus Require Antibiotics?

Learn how mucus color and consistency can indicate infections and when antibiotics may be necessary, helping you understand your health better.
When you're unwell, your body produces more phlegm, which may change in thickness and color. Mucus, also called snot, sputum, catarrh, or boogers, can be white, green, yellow, brown, or even black. Recognizing what these colors indicate can help determine whether you might need antibiotics or if the condition is viral or due to other causes.
What is mucus?
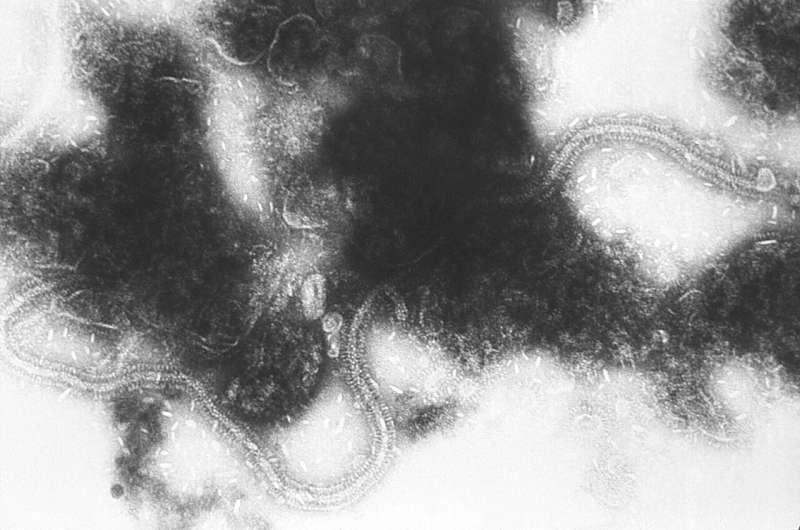
Mucus is a protective barrier produced by cells lining organs such as the respiratory, digestive, and ocular systems. Its primary functions are to lubricate tissues, trap dust, allergens, and bacteria, and contain antimicrobial molecules that combat pathogens.
Why does mucus increase during illness?
When your body detects pathogens like bacteria or viruses, your immune system triggers inflammation, causing the epithelial cells to produce more mucus. This hypersecretion aids in trapping and eliminating invaders. The tiny hair-like cilia in your airways help move mucus out, but infections or allergies can damage these cilia, making it necessary to cough or blow your nose to clear the buildup.
How does mucus thickness change?
Healthy mucus is mostly water, making it clear and runny. During illness, increased production of mucin proteins causes mucus to thicken, leading to congestion, post-nasal drip, and cough. Thickened mucus can trap more debris but also make breathing more difficult.
What does mucus color tell us?
- White or cloudy mucus often indicates early infection or inflammation from allergies.
- Green or yellow mucus suggests immune activity, as enzymes like myeloperoxidase are produced by immune cells fighting infection.
- Brown mucus may contain blood from irritated nasal passages.
- Black mucus is rare and could signal fungal infection or exposure to pollutants.
- Blood-tinged mucus warrants medical attention, especially if coughed up from the lungs.
Do I need antibiotics?
Medical professionals evaluate mucus characteristics along with other symptoms such as fever, fatigue, and duration of illness to decide on treatment. While yellowish-green mucus can sometimes indicate bacterial infection, this isn't always the case. The color alone isn't definitive for bacterial versus viral origin. Overuse of antibiotics can be ineffective or harmful if misapplied.
When to consult a healthcare provider
If you produce excessive mucus with changing color or consistency, especially if accompanied by prolonged symptoms like fever, fatigue, or loss of appetite, seek medical advice. Management strategies can include hydration, decongestants, and symptom relief. Antibiotics are reserved for confirmed bacterial infections, as determined by a healthcare professional.
Understanding mucus characteristics can help you better interpret your body's signals. However, consulting a healthcare provider is essential for accurate diagnosis and appropriate treatment.
For more detailed information, visit: https://medicalxpress.com/news/2025-07-yellow-mucus-antibiotics-phlegm-health.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
U.S. Panel Endorses New RSV Antibody Treatment for Children Amid Administrative Changes
An advisory panel has recommended a new antibody treatment for RSV in infants, marking a significant step in pediatric respiratory illness prevention amidst recent public health leadership changes.
Innovative 3D Bioprinted Mini Placentas Could Revolutionize Pregnancy Research
A pioneering study from UTS introduces 3D bioprinted placental organoids, offering a novel and precise model to study pregnancy complications such as preeclampsia, potentially transforming prenatal medicine.