Understanding What an IBD Diagnosis Means and Its Implications
Learn about Inflammatory Bowel Disease (IBD), its symptoms, diagnostic processes, and treatment options to better understand this chronic condition affecting the digestive system.
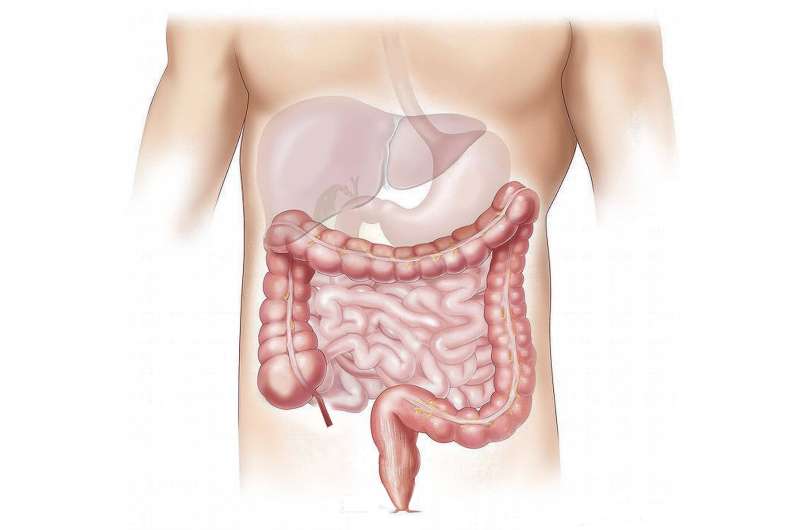
Inflammatory Bowel Disease (IBD) is a term used to describe a group of chronic conditions characterized by inflammation and swelling in the digestive tract. The two main types of IBD are ulcerative colitis and Crohn's disease, each affecting different parts of the gastrointestinal (GI) system and exhibiting distinct behaviors over time.
Ulcerative colitis primarily involves inflammation of the colon and rectum, leading to ulcer formation, bleeding, and symptoms such as abdominal pain, diarrhea, and fatigue. Crohn's disease, on the other hand, can affect any part of the GI tract from the mouth to the anus, often involving the small intestine, and may cause symptoms like weight loss, pain, and fatigue. While some individuals experience mild symptoms, others may face severe, life-threatening complications.
Diagnosing IBD involves a comprehensive process including medical history, symptom assessment, and various tests. Blood tests can identify signs of inflammation, anemia, or infections. Stool studies help rule out infections and detect markers of inflammation. Endoscopic procedures, such as colonoscopy and flexible sigmoidoscopy, enable visualization of the bowel and allow biopsy collection for definitive diagnosis. Advanced imaging techniques like capsule endoscopy and balloon-assisted enteroscopy help examine deeper parts of the small intestine.
Treatment usually begins with medications, including anti-inflammatory drugs, immune suppressors, and biologics targeting immune pathways to manage inflammation and symptoms. Surgery might become necessary if medications are ineffective, not tolerated, or complications develop. For ulcerative colitis, a colectomy (removal of the colon and rectum) may be performed, often with the construction of an internal pouch that allows waste to pass normally, or a permanent ileostomy if an internal pouch isn't feasible.
In Crohn's disease, surgery typically involves removing damaged segments of the digestive tract and reconnecting healthy tissue, with the aim to preserve as much healthy bowel as possible. Surgical intervention is tailored to the individual's condition and is influenced by factors such as disease severity, response to treatment, overall health, and personal preferences. Emergency surgeries may be necessary in urgent cases like perforation or severe bleeding.
Understanding IBD and its management options is essential for patients to make informed decisions in collaboration with their healthcare team. Managing IBD effectively can significantly improve quality of life, reduce symptoms, and prevent serious complications.
Source: https://medicalxpress.com/news/2025-08-ibd-diagnosis.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Key Mechanism Identified That Shields SARS-CoV-2 During Replication
Researchers have identified a vital mechanism that SARS-CoV-2 uses to protect its spike protein during replication, offering new targets for antiviral therapies and vaccine development.
Enhanced Technique Improves Precision of Blood Measurement Using Near-Infrared Spectroscopy
A new integrated approach significantly improves the accuracy of blood hemoglobin measurement using near-infrared spectroscopy, paving the way for non-invasive diagnostics.
Promising Drug Combination for Early Post-Myocardial Infarction Treatment
A pioneering preclinical study reveals that combining empagliflozin with sacubitril/valsartan could enhance early healing and reduce complications after a heart attack, paving the way for new treatment strategies.
Trends in Prescription Stimulant Use for ADHD Among U.S. Teens from 2005 to 2023
An analysis of U.S. adolescent stimulant use from 2005 to 2023 shows rising medical prescriptions for ADHD and a decline in nonmedical use, emphasizing the importance of ongoing monitoring.



