'Skin in a syringe': Breakthrough in Injectable Cell Technology for Wound Healing

Innovative research introduces a gel containing live cells that can be injected and 3D printed into skin transplants, offering new hope for wound healing and tissue regeneration.
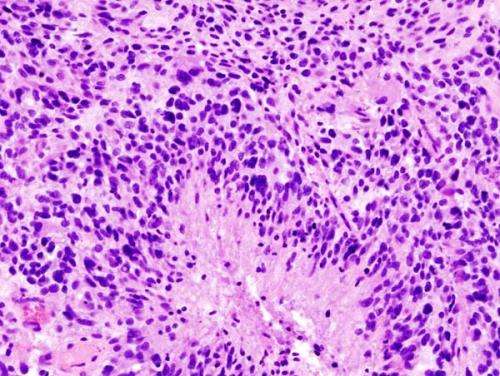
Researchers have pioneered a revolutionary approach to wound treatment by developing a gel containing living cells that can be 3D printed directly into skin transplants, a method dubbed "skin in a syringe." This innovative technology was demonstrated in studies conducted on mice and shows promise for treating burns and severe wounds more effectively. The team, led by the Center for Disaster Medicine and Traumatology in collaboration with Linköping University in Sweden, created a biocompatible gel made from a combination of gelatin beads and hyaluronic acid, which can be injected into wounds and then solidify into a supportive matrix. The gel particles are embedded with dermal cells, particularly fibroblasts, which are essential for forming the dermis—the deeper and more complex layer of skin that contains blood vessels, nerves, and hair follicles.
The process involves mixing the gelatin beads with a light-sensitive gel that becomes liquid under pressure but quickly re-solidifies once in place, allowing precise application via syringe. The research team successfully 3D printed small grafts from this material, which, when implanted in mice, not only survived but also promoted blood vessel formation and new tissue growth. This approach aims to bypass the challenges of growing full dermal layers in the lab, enabling the body to develop its structure naturally after the initial scaffold is transplanted.
In addition to skin regeneration, this technique holds potential for developing mini blood vessels and organoids—tiny, functional versions of organs—by creating perfusable channels within the hydrogel. The use of elastic, water-based hydrogel threads that can be manipulated into mini-tubes could lead to improved vascularization in engineered tissues, overcoming previous size limitations due to oxygen and nutrient diffusion constraints.
Overall, the "skin in a syringe" method presents a promising future for personalized regenerative medicine, providing a minimally invasive way to repair severe skin injuries while facilitating tissue growth and vascularization. The research underscores the potential to manufacture complex skin structures and blood vessels in the lab, bringing us closer to advanced treatments for burns, trauma, and possibly other tissue regeneration applications.
Source: MedicalXpress
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Wildfires and Their Impact on Increasing Risks of Flu and COVID-19 Spread
Wildfires may increase the risk of flu and COVID-19 outbreaks by driving more people indoors, where airborne diseases can spread more easily. Wearing masks can help reduce this risk during wildfire seasons.
Significant Survival Benefits in Glioblastoma Patients Using Proton Therapy: Findings from Recent Clinical Trial
Recent clinical trial results highlight the potential of proton therapy to improve survival in glioblastoma patients, offering hope for more effective, less toxic treatment options.
Do People Truly Want to Know Their Risk of Developing Alzheimer's?
A new study explores the emotional and ethical complexities of disclosing Alzheimer's risk, revealing many individuals prefer not to know their potential future, highlighting the need for careful consideration of testing practices.