Semaglutide Shows Promise in Improving Metabolic and Physical Health in Patients with Schizophrenia on Antipsychotics

A recent Danish study finds that weekly semaglutide improves blood sugar, promotes weight loss, and enhances physical health in adults with schizophrenia on antipsychotics, highlighting its potential as a safe and effective treatment option.
A collaborative study conducted by Danish researchers has revealed that weekly administration of semaglutide over a period of 30 weeks can significantly improve both metabolic and physical health outcomes in adults with schizophrenia who are undergoing treatment with second-generation antipsychotics. The study, published in JAMA Psychiatry, focused on patients with prediabetes and obesity—common comorbidities linked to antipsychotic medication use.
The randomized, double-blind clinical trial involved 154 participants aged 18 to 60 years, with 141 completing the full 30-week intervention. Participants received either semaglutide or a placebo once a week, with medication titrated to a maximum dose of 1.0 mg. Most assessments and visits took place in participants' homes, ensuring convenience and real-world applicability.
Results demonstrated a notable reduction in blood sugar levels, with HbA1c decreasing by 0.46% compared to the placebo group. Remarkably, 81% of those treated with semaglutide achieved HbA1c levels below 5.7%, indicating improved glycemic control. Additionally, participants experienced significant weight loss of approximately 9.2 kilograms, alongside improvements in lipid profiles—HDL cholesterol increased by 10.81 mg/dL and triglycerides decreased by 29.20 mg/dL.
Physical quality of life improved, with scores increasing by 3.75 points, although mental health outcomes and schizophrenia symptom severity, measured via PANSS-6, showed no substantial change. Gastrointestinal symptoms, commonly associated with GLP-1 receptor agonists, were more frequent early in treatment but tended to lessen over time, and serious adverse effects did not differ between the treatment and placebo groups.
The study's authors concluded that weekly semaglutide at the dose of 1.0 mg is a safe and effective option to improve glycemic control, promote weight loss, and enhance physical well-being in patients with schizophrenia receiving antipsychotics. These findings point toward the potential of semaglutide as a candidate therapy capable of addressing the metabolic side effects commonly seen with second-generation antipsychotics, thereby offering a dual benefit of improving physical health without compromising psychiatric stability.
This research underscores the importance of exploring new pharmacological strategies to mitigate cardiometabolic risks in psychiatric populations, potentially reducing the burden of premature morbidity and mortality associated with schizophrenia treatment.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
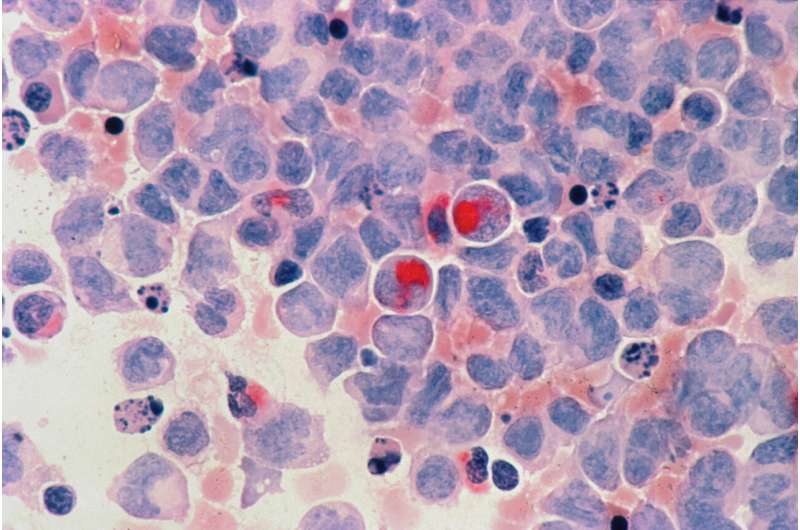
Genetic Mutations and Cell Maturity Key Factors in Overcoming Treatment Resistance in Acute Myeloid Leukemia
Recent research uncovers how gene mutations and cell maturity influence treatment resistance in acute myeloid leukemia, paving the way for personalized therapies and improved patient outcomes.
Astrocyte Protein RTP801 Implicated in Cognitive Decline in Alzheimer's Disease
New research reveals the role of astrocytic RTP801 protein in Alzheimer's disease, highlighting potential therapeutic targets to combat cognitive decline and neuroinflammation.
Innovative Approach: Simultaneous Kidney and Stem Cell Transplants Could Eliminate Long-Term Immunosuppressant Use
New research from Mayo Clinic demonstrates that simultaneous kidney and stem cell transplants may allow patients to live without lifelong immunosuppressive medications, offering hope for safer, longer-lasting transplants.
Artificial Intelligence Develops Two Novel Antibiotics Against Drug-Resistant Superbugs
MIT researchers have used AI to design two new antibiotics targeting resistant superbugs, marking a promising advancement in overcoming antimicrobial resistance. While further testing is needed, this innovative approach could transform future infectious disease treatments.