Rethinking COPD Diagnosis to Enhance Accuracy and Facilitate Early Detection
A new multidimensional diagnostic approach for COPD integrates symptoms and imaging data, enabling earlier and more accurate detection of at-risk individuals beyond traditional spirometry methods.
Recent research led by the University of Alabama at Birmingham has introduced a refined framework for diagnosing chronic obstructive pulmonary disease (COPD), emphasizing a more comprehensive approach to identify individuals at risk for severe respiratory issues who might be overlooked by traditional methods.
Globally, COPD affects approximately 392 million people and remains one of the leading causes of disability and death. Conventional diagnosis predominantly relies on spirometry, specifically measuring airflow obstruction through the forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) ratio, with a threshold of below 0.70 indicating COPD. However, numerous studies have highlighted that this approach often fails to detect significant structural lung abnormalities or symptoms in patients who do not meet this cutoff.
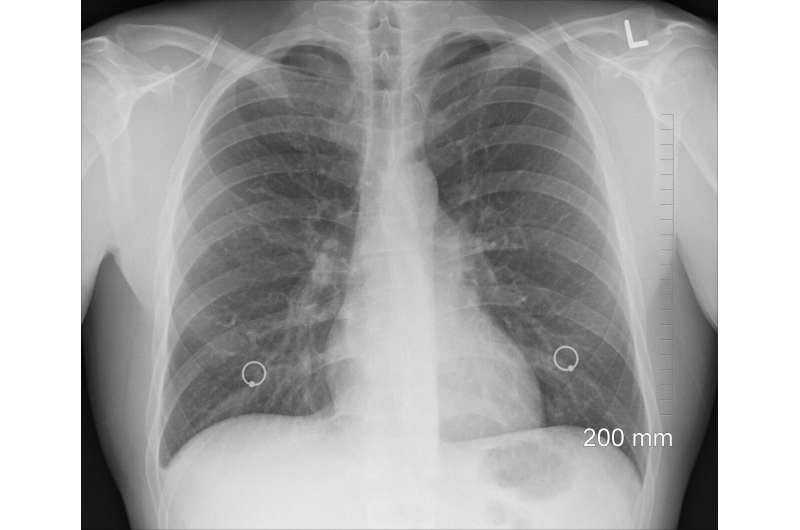
Imaging studies, such as chest CT scans, have demonstrated that individuals without airflow obstruction can still experience emphysema or bronchial wall thickening. Many of these patients, especially those with a history of smoking, report respiratory symptoms and report reduced quality of life, despite not fitting the traditional spirometric criteria.
Current guidelines acknowledge the importance of symptoms and imaging results but do not integrate these findings into a unified diagnostic model. There has been a call for a multidimensional approach that considers a broader array of clinical features.
In a recent study published in JAMA, researchers evaluated whether a diagnostic model incorporating respiratory symptoms and chest CT findings could better identify COPD cases and predict adverse outcomes. The study included two major cohorts: COPDGene in the United States with over 10,000 participants followed from 2007 to 2022, and CanCOLD in Canada with more than 1,500 participants followed through 2023.
Participants underwent spirometry and chest CT imaging. The proposed diagnostic framework utilized two pathways: a major category based on spirometry showing airflow obstruction plus at least one minor criterion (such as emphysema or airway wall thickening), and a minor category requiring three out of five minor criteria including emphysema, bronchial thickening, dyspnea, chronic bronchitis, and poor respiratory quality of life.
Results revealed that in the COPDGene cohort, 811 individuals without airflow obstruction were newly identified as having COPD due to minor criteria alone. These individuals faced higher risks of mortality—both overall and respiratory-specific—as well as more frequent exacerbations and faster decline in lung function, compared to those without COPD.
Similarly, in the Canadian cohort, a notable percentage of individuals without airflow obstruction were reclassified as having COPD based on additional clinical findings. While their overall mortality did not significantly differ, they exhibited increased exacerbation rates.
The study suggests that structural lung abnormalities and respiratory symptoms can predict worse outcomes even when spirometry appears normal. Such a multidimensional schema underscores the importance of integrating imaging and symptomatic assessments into COPD diagnosis, potentially leading to earlier intervention and better health equity, particularly among underdiagnosed populations like Black individuals.
This innovative approach may transform how clinicians identify and manage COPD, especially in early or atypical cases, ultimately improving patient outcomes and reducing the global burden of the disease.
Source: https://medicalxpress.com/news/2025-05-rethinking-copd-diagnosis-accuracy-early.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
COVID Resurgence in California: What the Summer Holds
California is experiencing a COVID resurgence this summer, with regional and wastewater data indicating rising infections. Experts warn to remain vigilant and get vaccinated to mitigate the impact of the potential wave.
Study Confirms Benefits of Shunt Surgery for Older Adults with Hydrocephalus
A recent clinical trial confirms that shunt surgery offers significant symptom relief for older adults with idiopathic normal pressure hydrocephalus, improving mobility and quality of life.
Regular Exercise May Slow Brain Degeneration in Parkinson's Disease
Regular physical activity is associated with slower brain degeneration and cognitive decline in early Parkinson's disease, offering potential neuroprotective benefits.
Implications of Medicaid Cuts for Americans Over 65: Insights from Aging Experts
Recent Medicaid funding cuts pose serious risks for Americans over 65, threatening access to care and increasing health disparities. Experts warn of widespread health and mortality consequences.



