Pulmonary Embolism in Children: A Growing Concern Recognized by New Research

New research reveals that pulmonary embolism in children is more common than previously believed. A large study highlights the need for increased awareness and updated diagnostic criteria in pediatric care.
Recent groundbreaking research has illuminated that pulmonary embolism (PE) in children is far more common than previously understood. Traditionally considered a rare condition in pediatric populations, emerging evidence now indicates that PE may occur as frequently in children as it does in adults, prompting a significant shift in clinical awareness and diagnostic approaches.
The pivotal study, published in the American Journal of Respiratory and Critical Care Medicine and presented at the ATS 2025 International Conference, analyzed data from over 4,000 children aged 4 to 17 presenting with symptoms suggestive of PE across 21 U.S. emergency departments. The findings revealed that approximately 6.3% of these children were diagnosed with acute pulmonary embolism, including those with isolated PE, deep vein thrombosis, or both conditions. These rates challenge previous estimates derived from retrospective studies, which suggested PE was exceedingly rare in children.
First author Dr. Jeffrey A. Kline emphasizes that PE should now be considered a differential diagnosis in adolescents with unexplained shortness of breath. The study also identified that the clinical patterns used to diagnose PE in adults are largely applicable to children, which aids in early recognition.
In terms of diagnostics, nearly 80% of the children underwent D-dimer blood testing, a marker for blood clots, followed by imaging studies such as CT pulmonary angiography, VQ scans, MRI, or venous ultrasounds to confirm the diagnosis. Importantly, the study proposes evidence-based criteria to guide clinicians in suspecting and testing for PE, aiming to reduce unnecessary radiation exposure.
This research raises critical questions: Are some children experiencing undiagnosed PE and recovering without intervention? Or are these conditions being missed, leading to long-term complications like pulmonary hypertension or even sudden death? The authors plan further multicenter studies to refine guidelines and evaluate the safety of ruling out PE without extensive testing.
This evolving understanding underscores the importance of increased vigilance and updated diagnostic protocols in pediatric care. Recognizing PE early can significantly influence treatment decisions and outcomes, highlighting a need for clinicians to consider this diagnosis more readily in symptomatic children.
Source: https://medicalxpress.com/news/2025-05-pulmonary-embolism-children-common-previously.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
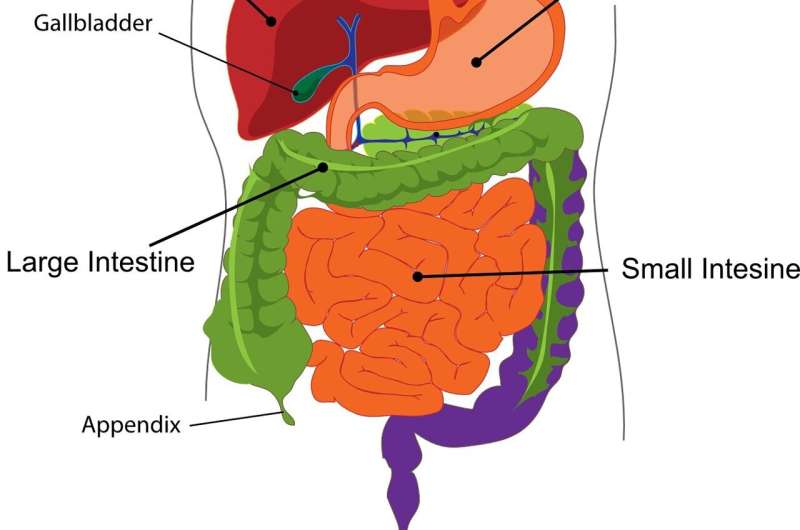
Bindi Irwin Undergoes Emergency Appendectomy: Understanding Appendicitis
Bindi Irwin recently underwent emergency appendectomy due to a ruptured appendix. Learn about appendicitis, its symptoms, and treatment options to understand this common condition better.
Innovative Bioprinted Organoids Enable Tumor Feature Capture and Prognosis Prediction
A novel 3D bioprinted tumor model combines patient-derived organoids with AI to accurately capture tumor features and predict patient prognosis, advancing personalized cancer treatment strategies.
FDA Accelerates Drug Approvals for Projects Supporting U.S. National Priorities
The FDA introduces a new fast-track program to streamline drug approvals for treatments that support U.S. health priorities, reducing review times from over a year to just a few months.