New Insights into Cocaine Use Disorder and Potential Therapeutic Approaches
Researchers at Virginia Commonwealth University have identified a molecular mechanism in the brain that offers a new target for developing medications to treat cocaine use disorder, focusing on dopamine regulation and receptor interactions.
A research team led by Virginia Commonwealth University has unveiled important molecular mechanisms underlying cocaine use disorder, highlighting a promising therapeutic target to mitigate the drug's addictive effects. Their study focused on how cocaine influences dopamine regulation in the brain—a critical factor in addiction. By modulating one specific component that governs dopamine levels, researchers were able to block the pathway reinforcing cocaine-seeking behaviors. Published in The Journal of Neuroscience, these findings open doors to developing medications that could help individuals overcome cocaine dependence.
Cocaine and other stimulant drugs such as methamphetamine are involved in about half of all overdose deaths in the United States, either alone or combined with opioids. Despite the availability of treatments for other substance use disorders like opioids and alcohol, there are no approved medications specifically targeting stimulant drug abuse. Experts emphasize the need for effective pharmacological interventions, as current understanding of cocaine's neurobiology remains incomplete.
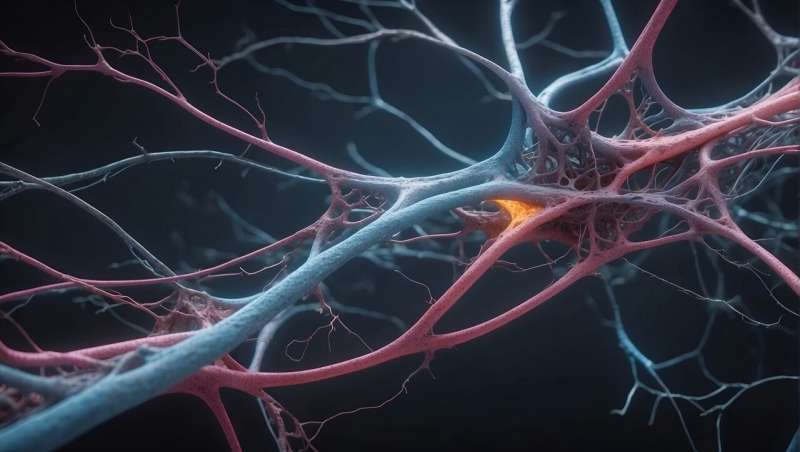
Research pioneers Dr. Lankupalle Jayanthi and Dr. Sammanda Ramamoorthy have been studying cocaine’s impact on the brain’s dopamine system for over 25 years. Dopamine, a neurotransmitter associated with pleasure and reward, gets hijacked by cocaine, causing an initial intense euphoria. Chronic use depletes dopamine, leading to dissatisfaction and increased drug-seeking to compensate for this deficiency—fueling addiction.
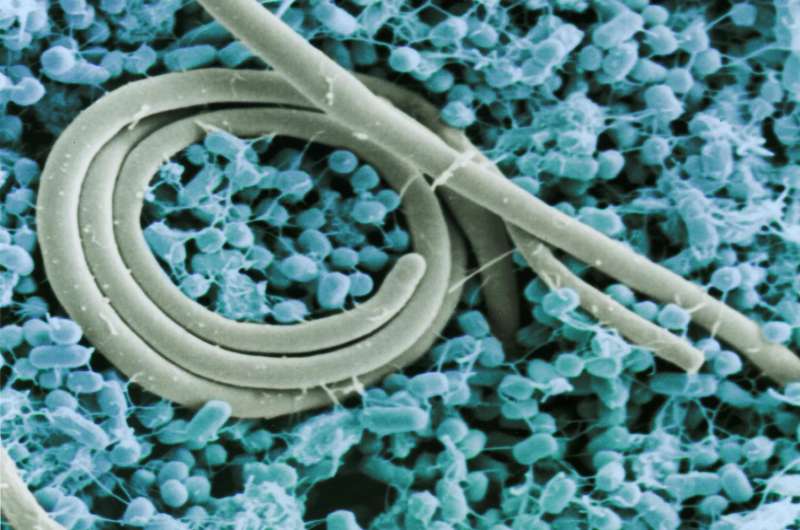
Cocaine targets two key proteins: kappa opioid receptors and dopamine transporters. The drug increases levels of dynorphin, activating kappa opioid receptors, which in turn make dopamine transporters overactive—rapidly clearing dopamine from the brain and reducing its natural presence. This disrupts normal reward signals, creating negative feelings and prompting repeated drug use.
To counter this, researchers discovered that controlling the phosphorylation of dopamine transporters—specifically at the amino acid threonine-53—could prevent these overactive processes. They engineered a mouse model where this site was modified, disabling its phosphorylation. Results indicated that mice with the altered transporters did not show the typical effects of kappa receptor activation or increased transporter activity, suggesting a potential target for future drug development.
Currently, Dr. Jayanthi and Dr. Ramamoorthy are working on an innovative mRNA-based therapy—mini genes producing peptides that block threonine-53 phosphorylation—aiming to normalize dopamine levels and diminish cocaine’s impact. They believe this approach could lead to effective treatments for cocaine addiction, filling a critical gap in addiction medicine.
Their research also extends to other dopamine-related conditions such as ADHD, schizophrenia, bipolar disorder, and autism spectrum disorder, further underscoring the importance of understanding dopamine regulation for mental health. Their latest studies are paving the way for targeted therapies that address the root causes of drug dependence and related neuropsychiatric disorders.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Native Tribal Groups Declare Sovereignty Amid Federal Crackdown on Gender-Affirming Healthcare
Native American tribal communities are asserting sovereignty to protect LGBTQ+ rights and access to gender-affirming healthcare amidst federal and state restrictions, emphasizing cultural identity and health equity.
Promising New Vaccine Targets Typhoid and Salmonella Infections in First Human Trial
A new vaccine showing strong immune responses against typhoid and invasive Salmonella has proven safe in initial human trials, offering hope for effective disease prevention in endemic regions and beyond.
Study Finds Cannabis Use May Significantly Increase Risk of Developing Type 2 Diabetes
A new large-scale study reveals that cannabis use may nearly quadruple the risk of developing type 2 diabetes. Learn about the potential health implications of increasing cannabis consumption worldwide.
The Role of FGF21 Hormone in Reversing Fatty Liver Disease
New research shows that the hormone FGF21 can effectively reverse fatty liver disease by signaling the brain to improve liver health and reduce fibrosis, opening new therapeutic possibilities.