Postpartum Recovery: Navigating the Challenges Beyond Birth

New research introduces the Stanford Obstetric Recovery Checklist (STORK), a tool designed to assess physical, emotional, and social recovery in new mothers, promoting earlier intervention and better postpartum care.
Giving birth is often portrayed as a joyous milestone, with new parents proudly sharing photos of their newborns. However, behind these joyful images lies a complex reality—pain, fatigue, emotional upheaval, and the overwhelming process of recovery. Many new mothers focus heavily on the immediate challenges of caring for their infant, but often overlook their own physical and mental health as they leave the hospital.
Dr. Pervez Sultan, an obstetric anesthesiologist, recalls that when his wife delivered their first child, he thought he understood what to expect. Yet, he was surprised to find that postpartum recovery was not well described or standardized. This gap prompted him, along with colleagues at Stanford Medicine, to develop a new tool called the Stanford Obstetric Recovery Checklist (STORK). This comprehensive survey aims to assess a mother’s physical healing along with mental health, emotional well-being, social support, and sleep quality, enabling early detection of recovery issues.
Postpartum recovery is complex—women often face pain, bleeding, breastfeeding difficulties, hormonal shifts, social adjustments, and sleep deprivation. Additionally, nearly 20% of women may experience depression within the first year after birth. These challenges contribute to an increased risk of maternal complications and even death after leaving the hospital, highlighting the need for better assessment and support.
Currently, postpartum checkups happen at about six weeks, but by then, some issues may have become severe or unrecognized. The STORK tool offers a standardized method to evaluate recovery across multiple domains during routine postpartum visits. It uses 47 straightforward questions to identify problems such as mobility issues, emotional distress, anxiety, or lack of social support—factors critical to a mother’s health and well-being.
Research indicates that first-time mothers and those with infants admitted to neonatal intensive care tend to have a more difficult recovery. By collecting data early on, healthcare providers can predict which women may face extended challenges, allowing for timely interventions. The goal is to move toward earlier, more personalized postpartum support, possibly incorporating brief assessments two weeks after birth that could lead to comprehensive follow-up care involving obstetricians, mental health specialists, and lactation consultants.
Ultimately, this effort aims to improve postpartum care, reduce maternal mortality, and ensure that mothers receive the best possible support during one of the most vulnerable periods of their lives.
source: https://medicalxpress.com/news/2025-06-joy-birth-moms-wilderness.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
The Critical Role of Educating Children About Zoonotic Diseases and Safe Animal Interactions
Learn about the importance of teaching children safe interactions with animals to prevent zoonotic diseases and protect their health.
Low Cervical Cancer Screening Rates in Counties Linked to Higher Incidence and Mortality
Counties with persistently low cervical cancer screening rates face significantly higher rates of diagnosis and death. This study highlights the urgent need for improved screening access in underserved areas to reduce cervical cancer burden.
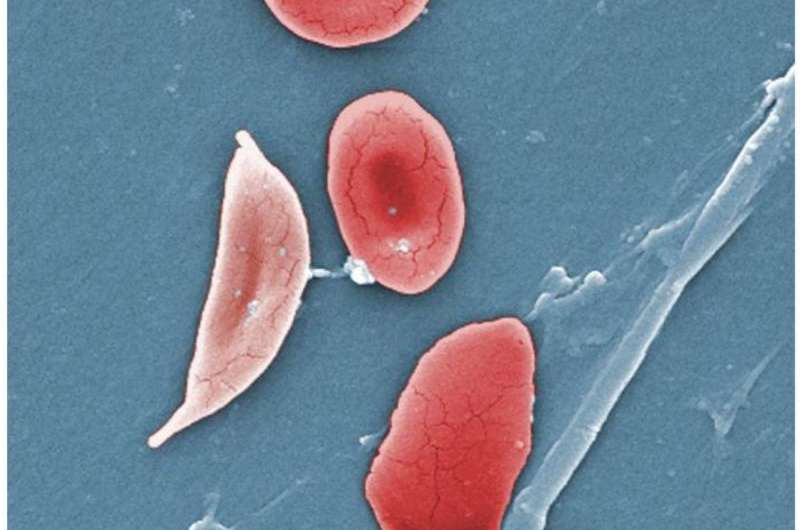
Innovative Treatment Algorithms Reduce Hospitalizations for Children with Sickle Cell Disease
Implementing standardized treatment algorithms for children with sickle cell disease at MUSC has led to a significant reduction in hospital stays while maintaining patient safety and improving quality of life. Discover how this collaborative approach is shaping future pediatric care.
Enhancing Road Safety Through Shared Responsibility and Innovation
A comprehensive approach involving shared responsibility and technological innovation is vital to reducing roadway fatalities and creating safer transportation systems for all road users.