Innovative Use of Patient Stem Cells Shows Promise for End-Stage Kidney Disease Treatment

Mayo Clinic researchers have shown that using a patient's own fat-derived stem cells can improve arteriovenous fistula healing in dialysis patients, offering new hope for end-stage kidney disease treatment.
Researchers at Mayo Clinic have uncovered promising results in the fight against end-stage kidney disease (ESKD) through the use of a patient’s own stem cells. In a recent study, transplanting mesenchymal stem cells derived from fat tissue into the veins of patients with arteriovenous fistulas (AVFs)—created surgically to facilitate dialysis—led to improved healing and increased durability of these blood vessels. This advancement could significantly extend the lifespan of AVFs, which are essential for hemodialysis, particularly considering that approximately 60% of AVFs fail due to vein narrowing.
End-stage kidney disease affects over 4 million people worldwide, with hemodialysis being a critical, yet temporary, treatment before a kidney transplant becomes necessary. The process involves connecting an artery and a vein in the arm to form an AVF, a crucial access point for dialysis. However, inflammation and vein narrowing pose substantial challenges, often leading to treatment failure. The researchers found that injecting patients with their own fat-derived stem cells mitigated inflammation, thereby promoting better healing of the AVF.
These adult mesenchymal stem cells secrete growth factors that aid in tissue repair and exhibit anti-inflammatory properties. Dr. Sanjay Misra, the senior author of the study, explained that inflammation is a common underlying factor in many health issues, including heart disease, vascular conditions, and cancer, making this therapy particularly valuable.
The clinical trial involved 21 participants, with 11 receiving stem cell injections prior to AVF surgery and 10 serving as a control group. Those who received stem cells experienced faster healing and more robust vessel maturation, although responses varied among individuals. Further analysis revealed specific genetic biomarkers associated with positive responses to stem cell therapy. These biomarkers could help predict which patients are most likely to benefit, paving the way for personalized treatment approaches.
The ongoing research includes preclinical models and advanced genetic analysis to optimize this therapy. Dr. Misra emphasized that if larger clinical trials validate these findings, this approach could transform treatment options, reduce healthcare costs, and set new guidelines for managing dialysis access in kidney failure patients.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Innovative Tool Developed to Detect Untrustworthy Research Trials
Researchers introduce INSPECT-SR, a groundbreaking tool designed to identify unreliable and fraudulent research trials, enhancing the integrity of medical evidence and systematic reviews.
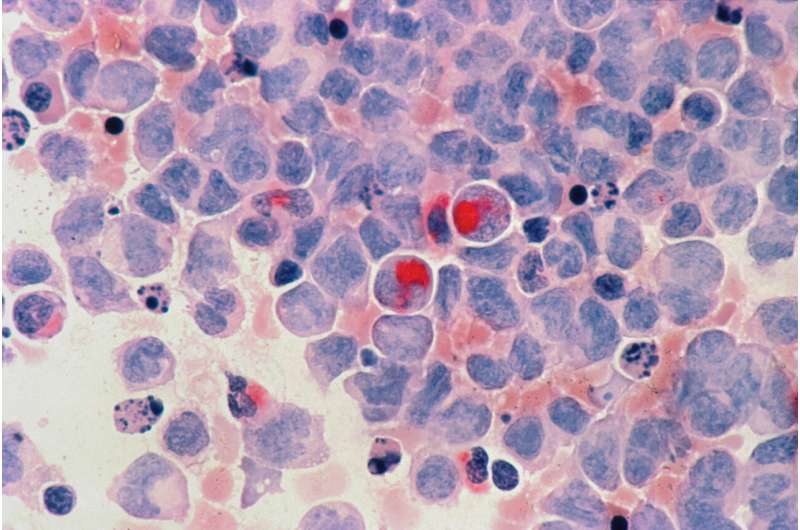
Genetic Mutations and Cell Maturity Key Factors in Overcoming Treatment Resistance in Acute Myeloid Leukemia
Recent research uncovers how gene mutations and cell maturity influence treatment resistance in acute myeloid leukemia, paving the way for personalized therapies and improved patient outcomes.
Recall Issued for Bariatric Fusion Vitamins Due to Missing Child-Safe Caps
A recall has been issued for Bariatric Fusion multivitamins due to packaging lacking child-resistant caps, preventing potential accidental iron poisoning in children. Consumers are urged to act immediately.