Multicenter Study Demonstrates Effectiveness of Near-Infrared Autofluorescence in Detecting Parathyroid Glands

A large multicenter trial confirms that near-infrared autofluorescence technology greatly improves the detection of parathyroid glands during neck surgery, reducing risks and enhancing surgical precision.
A comprehensive multicenter clinical trial led by Vanderbilt University and Vanderbilt University Medical Center has provided compelling evidence that near-infrared autofluorescence (NIRAF) technology significantly enhances the intraoperative identification of parathyroid glands (PGs). This advancement is particularly important during endocrine neck surgeries such as thyroidectomy and parathyroidectomy, where accurate localization of PGs is critical to prevent postoperative complications like hypoparathyroidism.
The study involved 752 patients undergoing surgery for hyperthyroidism or thyroid disease across four major medical centers, including Vanderbilt, the University of Michigan, UC-San Francisco, and the Medical College of Wisconsin-Milwaukee. The trial assessed the use of a device incorporating the FDA-approved PTeye probe, developed by Vanderbilt’s Biophotonics Center, which emits fluorescence signals emitted by PG tissue. This device leverages the property that parathyroid tissue naturally fluoresces more intensely in the near-infrared range compared to surrounding tissues, allowing surgeons to identify glands with high precision.
Results showed a notable increase in the number of PGs detected when using the NIRAF device. For bilateral procedures, the average number of glands identified rose from 3.2 to 3.5, while during thyroidectomies, the count increased from 2.8 to 3.3. Importantly, the technology did not significantly alter the rates of transient or long-term hypoparathyroidism, indicating its safety and potential to improve surgical outcomes.
The device's development was driven by Vanderbilt's efforts to translate laboratory findings into clinical practice. Dr. Anita Mahadevan-Jansen explained that PGs emit a stronger autofluorescence signal than other neck tissues, enabling their glow during surgery. This capability facilitates more accurate and efficient gland detection, reducing the risk of inadvertent damage or removal.
While normal PGs are small and often indistinguishable from adjacent tissues, the use of NIRAF technology has demonstrated an accuracy rate of approximately 97% in detecting these glands, surpassing traditional visual identification methods. Dr. Carmen Solórzano emphasized that PGs can be located anywhere from below the jaw to the chest, underscoring the importance of advanced imaging tools in surgery.
This trial marks a significant advancement toward integrating autofluorescence technology into standard endocrine surgery protocols, ultimately aiming to improve patient outcomes by minimizing complications associated with gland misidentification.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Nasal Mask Support Enhances Breathing Outcomes in Preterm Infants: Landmark Clinical Trial
A major clinical trial reveals that nasal mask support at birth significantly improves breathing in extremely preterm babies, potentially transforming neonatal resuscitation practices worldwide.
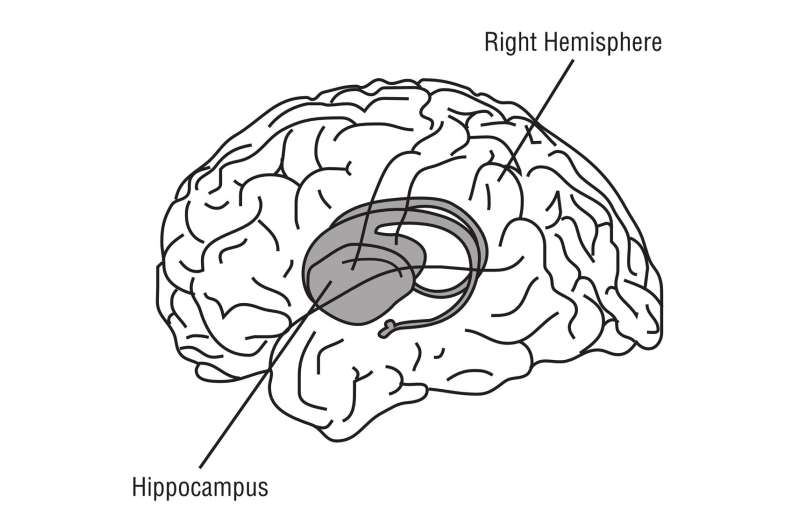
Adult Brain Continues Neurogenesis in the Hippocampus: New Research Findings
New research demonstrates that the human hippocampus continues to produce new neurons throughout adulthood, revealing exciting possibilities for brain health and regenerative therapies.
Understanding the Hidden Food Safety Risks at Buffets and How to Protect Yourself
Buffet dining offers variety but poses significant health risks due to cross-contamination, temperature issues, and allergens. Learn how to stay safe and enjoy your meal responsibly.
Promising Results of Combined Epigenetic Therapy in Blood Cancer Treatment
A groundbreaking preclinical study shows that combined epigenetic inhibitors targeting G9a and DNMTs can effectively reduce tumor growth and induce cell death in multiple myeloma, opening new therapeutic possibilities.