Survey Highlights Persistent Misconceptions About Hormone Therapy Use in Gynecologic Cancer Patients
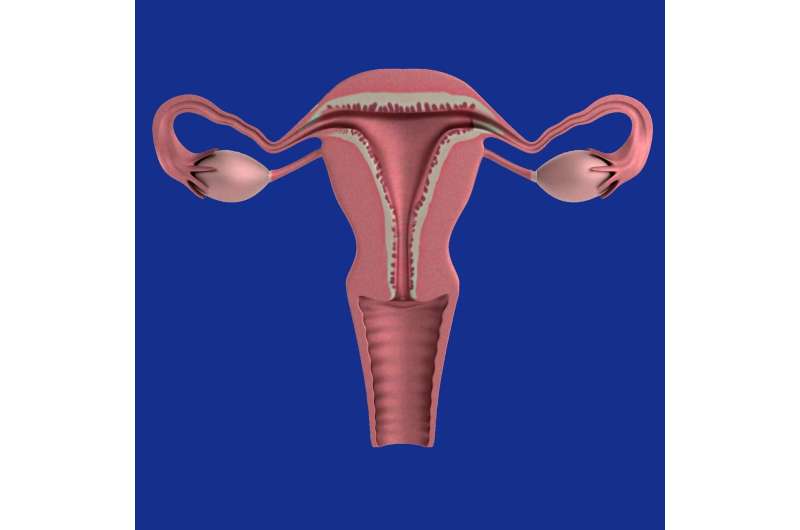
Despite evidence supporting safety, misconceptions prevent many healthcare providers from prescribing hormone therapy to gynecologic cancer patients. A new survey highlights the need for better education to optimize patient care and quality of life.
Recent research reveals that misconceptions among healthcare providers continue to hinder the appropriate use of hormone therapy in patients with gynecologic cancers. Despite substantial evidence supporting the safety of hormone therapy for individuals with a history of low-grade endometrial or epithelial ovarian cancer, many gynecologists and some gynecologic oncologists remain hesitant to prescribe it. This reluctance underscores the need for enhanced clinician education to dispel myths and misconceptions.
A survey published in the journal Menopause investigated the prescribing habits and beliefs of 293 healthcare professionals, including members of the Society of Gynecologic Oncology (SGO) and the American College of Obstetricians and Gynecologists. The results indicated that while 63.82% of respondents prescribe estrogen therapy to patients with endometrial cancer, and 65.19% feel comfortable prescribing it to those with epithelial ovarian cancer, a significant proportion nonetheless harbor concerns. Notably, 96.8% are comfortable prescribing estrogen for cervical cancer patients.
The survey also revealed variations in prescribing patterns based on factors such as sex, job title, and clinical experience. Less experienced practitioners and those specializing in benign gynecology are more likely to hold misconceptions about hormone safety. Additionally, most providers prefer alternative therapies like selective serotonin reuptake inhibitors (88.4%), gabapentin (58%), and neurokinin-3 antagonists (46.4%) for managing menopausal symptoms.
Hormone therapy remains one of the most effective treatments for menopausal vasomotor symptoms and genitourinary syndrome, significantly improving quality of life. The hesitation to prescribe it often stems from the erroneous belief that the risks outweigh benefits—a notion that is increasingly being challenged by current research. Dr. Monica Christmas of The Menopause Society emphasizes that understanding when hormone therapy can be safely used can lead to better outcomes for women post-gynecologic cancer treatment.
The study highlights a vital gap in education and practice, underscoring the importance of updating clinical guidelines and training to ensure patients receive evidence-based care. As treatments for gynecologic cancers improve and more women are cured or have prolonged survival, addressing misconceptions about hormone therapy becomes essential in comprehensive survivorship care.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Influence of Urban Design and Socioeconomic Factors on Dengue Hotspots in Medellín
A comprehensive study links urban design and socioeconomic disparities to dengue hotspots in Medellín, highlighting the need for targeted public health strategies to better control outbreaks and address underlying social inequalities.
The Rise of the Longevity Industry and Its Hidden Costs
Exploring the rise of the longevity industry and its promising claims about life extension, this article examines the scientific, ethical, and financial risks involved in pursuits of immortality.
Updated Recommendations: COVID-19 Vaccines No Longer Suggested for Healthy Children and Pregnant Women
In 2025, health authorities announced that COVID-19 vaccines are no longer routinely recommended for healthy children and pregnant women, shifting focus to high-risk groups amid evolving evidence and regulatory changes.



