Maternal Microbes Influence Early Brain Development, New Research Finds
Emerging research reveals that maternal microbes play a vital role in early brain development, affecting regions responsible for stress and social behavior, with implications for obstetric practices.
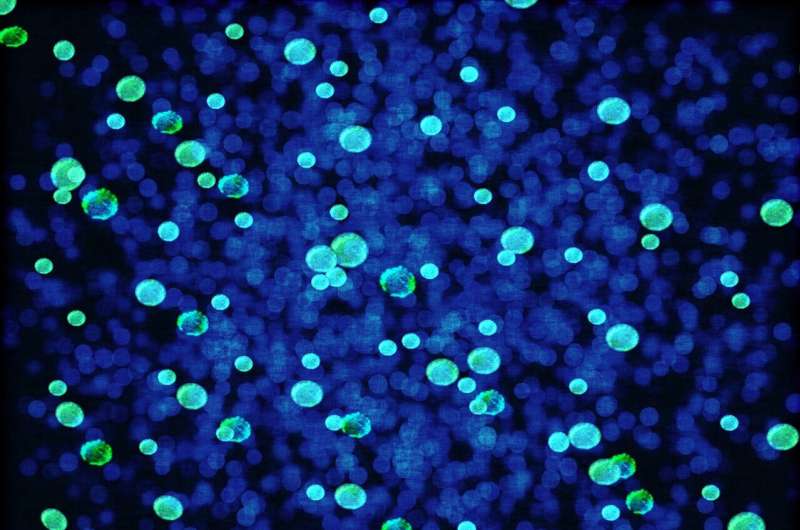
Recent research from Michigan State University highlights the crucial role that maternal microbes play in shaping early brain development. The study, published in the journal Hormones and Behavior, emphasizes how exposure to microbes during the perinatal period can impact critical brain regions responsible for stress regulation, social behavior, and vital bodily functions.
Using a mouse model, scientists demonstrated that microbial exposure immediately after birth influences brain structure development and possibly begins in the womb. Because mice share significant biological similarities with humans, they serve as an effective model for studying the influence of microbes on brain development. This research is especially relevant in the context of modern obstetric practices, such as antibiotic use during childbirth and cesarean sections, which can disrupt maternal microbial transmission. In the United States, about 40% of women receive antibiotics around childbirth, and approximately one-third of births occur via cesarean, potentially impacting the natural microbiome transfer.
Lead researcher Alexandra Castillo Ruiz explained that at birth, a baby is colonized by microbes as it passes through the birth canal—a process that coincides with key developmental events in the brain. Her team focused on a vital brain area called the paraventricular nucleus of the hypothalamus (PVN), which regulates stress responses, blood pressure, water balance, and social behaviors. Previous studies showed that germ-free mice, which lack microbes, presented with increased neuron death in the PVN during early development.
In experiments involving cross-fostering, germ-free newborn mice raised by microbe-rich mothers exhibited fewer neurons in the PVN shortly after birth, regardless of when microbes were introduced. Notably, adult germ-free mice also had reduced neuron numbers in this brain region. Dr. Castillo-Ruiz concluded that microbes are integral in shaping this essential brain area and that their effects may begin in the womb via signaling from maternal microbes. The findings underscore the importance of recognizing microbes as partners in early development, aiding in the construction of healthy brains from the very beginning.
This study advances our understanding of how maternal microbiomes influence neurodevelopment and highlights the potential long-term consequences of disrupting microbial transfer during delivery.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Innovative Open-Source Diagnostic Tool Enhances Affordable Pathogen Detection in Low-Resource Settings
A novel open-source RT-LAMP assay offers a cost-effective, heat-stable solution for pathogen detection in remote and resource-limited areas, advancing global health diagnostics.
Reforming the Process to Address Sexual Misconduct by UK Doctors: Experts Call for Major Changes
Experts call for major reforms in the UK’s system for addressing sexual misconduct by doctors to ensure fairer treatment, better victim support, and enhanced public trust.
Link Between Missing Y Chromosome Gene and Male Infertility Uncovered
Scientists at the University of Hawaiʻi at Mānoa have discovered that the absence of a specific Y chromosome gene, Zfy, causes male infertility by disrupting gene regulation and sperm development. This research provides valuable insights into the genetic causes of reproductive issues in men.
New Research Reveals Basal Stem-like Cells as the Origin of Small Cell Lung Cancer
A new study identifies basal stem-like cells as the origin of small cell lung cancer, highlighting new avenues for prevention and targeted treatment strategies.



