Understanding How Malaria Parasite Breaches the Brain's Defense in Cerebral Malaria

A groundbreaking study reveals how the malaria parasite breaches the blood-brain barrier, leading to cerebral malaria, and explores potential therapeutic interventions to prevent brain damage.
Cerebral malaria remains a severe and often fatal complication of malaria, particularly affecting children, with about 20% of affected children succumbing to the disease. Survivors frequently suffer from long-term disabilities. The causative agent, Plasmodium falciparum, reproduces within red blood cells and eventually and ruptures out, continuing its cycle of infection. A critical factor in the disease’s severity is its ability to compromise the blood-brain barrier (BBB), a protective structure that prevents harmful substances from entering the brain.
Recent research from EMBL Barcelona has provided significant insights into this process. The scientists developed a sophisticated laboratory model of the human BBB, plated with key cellular components such as endothelial cells, supporting pericytes, and astrocytes, arranged in a 3D structure with flowing fluids to mimic in vivo conditions. This 'BBB-on-a-chip' model allowed researchers to observe the effects of the parasite at its most active stage—when it exits red blood cells—a process known as egress.
Using live imaging techniques, the team tracked fluorescent molecules leaking through the barrier, demonstrating that infection and parasite egress increase BBB permeability significantly. Gene expression analysis at a single-cell level revealed a decrease in proteins essential for maintaining BBB integrity, alongside increased inflammation-related molecules. These findings delineate how Plasmodium falciparum damages the BBB, leading to leakage, swelling, and potentially irreversible brain damage.
Furthermore, the researchers tested the effects of Ruxolitinib, an FDA-approved drug that inhibits the JAK-STAT pathway involved in inflammation. The results showed that the drug could reduce BBB leakiness by calming inflammation and preventing fluid from seeping into the brain. This discovery points to potential therapeutic avenues for severe cases of cerebral malaria.
The study’s senior author, Maria Bernabeu, emphasized the next steps: incorporating immune cells and additional brain cell types like microglia and neurons into the model. This would create a more comprehensive simulation to better understand the disease mechanism. Overall, this research not only advances our understanding of how malaria damages the brain but also paves the way for developing targeted treatments to prevent long-term neurological damage in affected patients.
Source: https://medicalxpress.com/news/2025-09-cerebral-malaria-parasite-brain.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Innovative Imaging Technique Tracks Protein Alterations in Cancer Cells Without Dyes
A new non-invasive imaging method using mid-infrared light detects protein changes in cancer cells in real time, advancing personalized treatment assessments without dyes or labels.
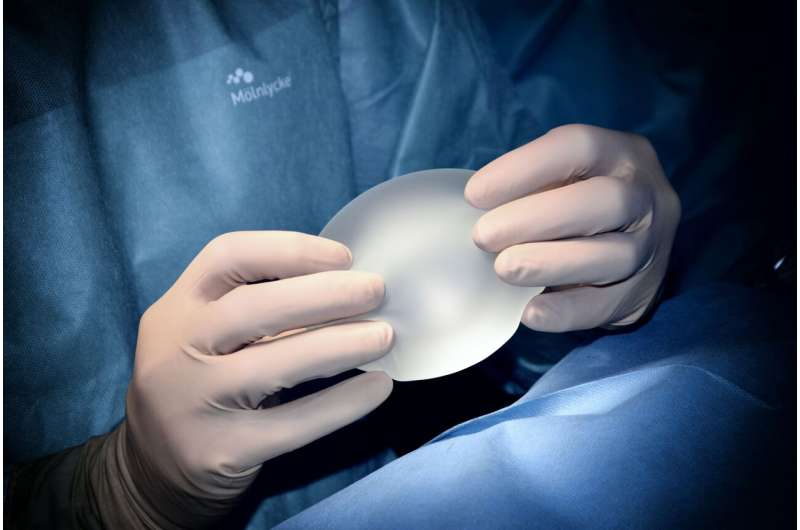
Increased Risk of Rare Lymphoma in Breast Cancer Patients with BRCA Mutations and Textured Implants
Women with breast cancer carrying BRCA mutations who receive textured breast implants face a significantly higher risk of developing rare lymphoma, according to new research. The study underscores the importance of genetic testing and personalized healthcare in breast reconstruction decisions.
Innovative Approach Uses Neutrophil Reprogramming to Combat Breast Cancer
A new study highlights how retraining neutrophils via innate immunity activation offers a promising therapeutic approach for difficult-to-treat breast cancers, including triple-negative subtypes.