Long-Term Risks of Type 2 Diabetes Linked to Zika Virus Infection
Research reveals that Zika virus can infect the hypothalamus in adults, leading to sustained insulin resistance and an increased risk of developing type 2 diabetes long after initial infection. This discovery broadens understanding of Zika’s long-term health impacts beyond fetal development concerns.
Since the world first encountered the Zika virus over a decade ago, researchers have been uncovering its complex impacts on human health. The initial alarm arose in 2015 when outbreaks in Brazil led to a surge in cases of microcephaly, a severe brain development disorder in newborns. Obstetrician Adriana Melo was among the first to connect Zika infections during pregnancy with fetal brain malformations after noticing abnormal ultrasounds. Her early investigations confirmed that Zika could cause significant developmental issues.
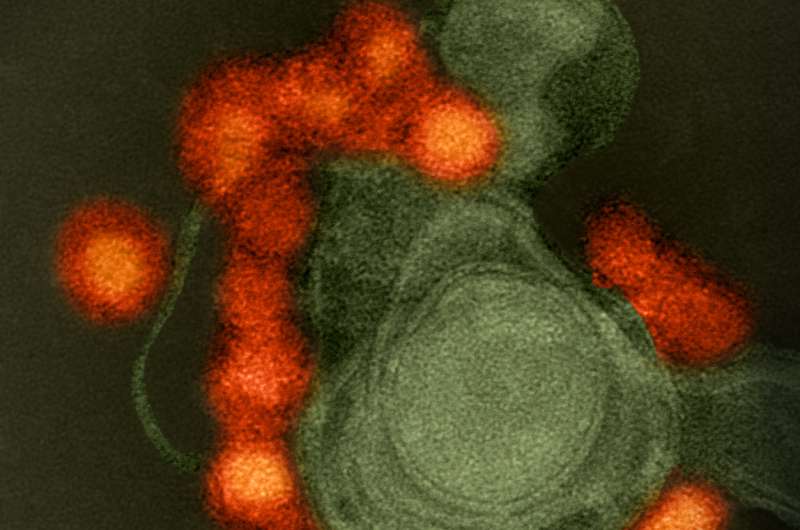
Over the years, scientific understanding of Zika's effects has broadened. Recent research highlights that the virus can also infect specific brain regions in adults, notably the hypothalamus—a critical area controlling hunger, temperature, and metabolism. Studies involving adult mice have demonstrated that Zika infection triggers brain inflammation, activates immune responses, and causes persistent insulin resistance. This disruption could increase the risk of long-term metabolic conditions such as type 2 diabetes, even after the initial infection has resolved.
In particular, Zika's ability to invade the hypothalamus leads to inflammation that hampers insulin function. This impairment hampers the body's capacity to regulate blood sugar levels effectively, which is a hallmark of type 2 diabetes. These findings were published in the journal Cell Death and Disease, emphasizing that Zika’s impact extends beyond fetal development concerns into adult health risks.
The research also indicates that Zika infection induces immune activation and hormone disruption that persists in the brain. This is consistent with observations of other viruses like dengue and influenza, which have been linked to long-term metabolic disturbances. The implication is clear: individuals who have experienced Zika infection might face heightened risks for metabolic illnesses later in life.
Understanding Zika's broader effects underscores the importance of ongoing surveillance of viral outbreaks and their long-term consequences. It suggests that managing Zika shouldn't solely focus on preventing congenital disabilities but also on monitoring potential adult health issues, including insulin resistance and type 2 diabetes. Continued research is vital to developing strategies that could mitigate these long-term risks and better prepare us for future viral threats.
Source: https://medicalxpress.com/news/2025-09-zika-virus-term-diabetes.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Radiation Therapy Might Promote Amphiregulin, Enhancing Metastatic Growth
Emerging studies indicate that radiation therapy may inadvertently promote metastasis by increasing amphiregulin levels, a factor that enhances tumor growth and spread. Exploring targeted interventions could improve therapeutic outcomes for patients with advanced tumors.
Innovative Silicone Models Revolutionize Medical Training and Research in Cerebral Vasculature
Swiss Vascular has developed detailed silicone models of cerebral blood vessels to improve medical training and reduce animal testing, advancing ethical research and clinical procedures.
Study Finds No Effect of Time-Restricted Eating on Sleep, Mood, or Quality of Life
A new study reveals that time-restricted eating does not negatively affect sleep, mood, or quality of life in adults with overweight or obesity, supporting its safety as a weight management strategy.
Innovative Space-Based Study Unveils New Insights into Alzheimer's Protein Aggregation
Space experiments aboard the ISS have enabled the detailed structural analysis of Alzheimer's-related amyloid β fibrils, revealing new pathways in disease progression and showcasing the crucial role of microgravity in biomedical research.



