The Limitations of Objective Pain Measurement Technologies

Exploring the challenges and philosophical considerations behind emerging objective pain measurement technologies, and their implications for pain management.
Pain assessment has traditionally relied on subjective reports, typically using a numerical scale from 0 to 10 or smiley faces for children, to gauge the intensity of a person's discomfort. While this approach has been the standard for decades, it presents significant limitations. Individuals interpret their pain differently; what one person rates as a five might be perceived as a three or eight by another, making standardization difficult.
Recent advancements in pain research suggest that we are nearing the development of objective pain measurement devices. These cutting-edge tools aim to quantify pain by analyzing biological markers—such as nerve fiber activity, pupil dilation, or blood flow variations—and comparing these patterns to extensive data from people experiencing pain. The promise is that such devices could revolutionize diagnosis, improve drug testing for analgesics, and streamline healthcare costs by providing more precise pain assessments.
However, a fundamental challenge remains. These devices are validated against subjective pain ratings, which are inherently unreliable due to individual differences in pain perception and reporting. The core issue is that pain is fundamentally a personal, subjective experience, accessible only to the individual experiencing it. Linking biomarkers to pain ratings does not necessarily provide a true, independent measure of pain but rather an indirect proxy based on correlations.
This philosophical dilemma raises questions about the actual accuracy and utility of these technologies. If an objective device produces the same pain score as a patient’s subjective rating, does it mean the measurement is truly more accurate? Or is it merely reflecting the same flawed self-report? Without understanding pain independently of personal perception, objective devices may not fully capture the complexity of pain experiences.
Ultimately, the development of these technologies highlights a crucial debate: can pain ever be fully quantified without subjective input? While the promise of objective measurement is enticing—potentially leading to better treatments and understanding—the intrinsic subjectivity of pain suggests that personal reports will continue to play a vital role in pain management. The key is to recognize the limitations of both subjective ratings and current biomarker-based techniques, and to approach pain assessment with a nuanced perspective.
Source: https://medicalxpress.com/news/2025-05-pain-score-problem.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Enhanced Eye Imaging Using AI Revolutionizes Diagnostic Accuracy
A new AI-driven approach utilizing physics-informed models significantly improves the clarity of eye images, aiding in more accurate diagnosis of ocular conditions.
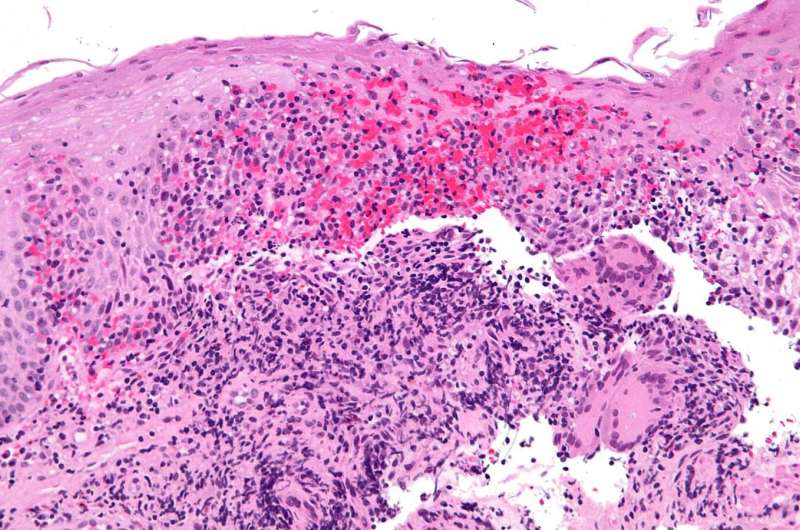
Reducing Inflammation to Protect Kidney Health in Lupus Nephritis
A groundbreaking approach to prevent kidney damage in lupus nephritis focuses on protecting blood vessel cells with targeted therapies, reducing inflammation without suppressing the immune system.
Strategies to Halt the Spread of HIV in the Southern United States
The Southern United States has become a new hotspot for HIV infections. Increased education, testing, and access to treatment are vital to curbing this growing epidemic. Learn more about effective strategies to stop HIV in the South.
Genetic Mutation Influences Iron Deficiency in Crohn's Disease Patients
A groundbreaking study reveals how genetic mutations in PTPN2 impair iron absorption, leading to anemia in Crohn's disease patients, paving the way for personalized therapies.