Insurers Contend with Rising Costs of GLP-1 Medications and Consider Patient Deprescription Strategies

Rising costs of GLP-1 medications lead insurers to restrict coverage and explore deprescription strategies, impacting patient care and weight management efforts.
In 2025, healthcare providers and insurers are grappling with the significant financial burden posed by GLP-1 receptor agonists, a class of medications including brands like Ozempic, Wegovy, Mounjaro, and Zepbound, primarily used for weight management and type 2 diabetes. As demand for these drugs surges, the high monthly costs—often around $1,000—are straining public and private payers, leading to restrictions and cancellations of coverage.
Patients like 25-year-old Kyra Wensley have experienced firsthand the impact of these policy shifts. After losing 50 pounds on Zepbound, Wensley's insurance denied coverage because her BMI was under the approved threshold at the start of treatment. Despite being effectively managed on the medication, she was required to switch to Wegovy, which she prefers less but remains on due to coverage constraints. Such restrictions highlight the growing trend of insurers limiting or ending GLP-1 coverage, including Medicaid programs in states like North Carolina and Pennsylvania, due to budget pressures.
Research indicates that many patients discontinue GLP-1 medications within a year, often because of side effects, costs, or insurance issues. To address this, medical professionals and policymakers are exploring "deprescription"—a strategy to taper off the medication after initial goals like weight loss are achieved. The UK’s National Institute for Health and Care Excellence recommends a two-year limit for some weight loss drugs, reflecting a broader consideration for time-limited use.
Advocates argue that deprescription could enable broader access by reallocating resources to more patients. For instance, some institutions like the University of Michigan cap GLP-1 coverage at two years when used solely for weight loss.
However, experts warn that weight often rebounds after stopping these medications, with many patients returning to previous weight levels. Currently, there is no standardized method for safely tapering off GLP-1s, complicating efforts. Yet, innovative approaches—like behavioral support programs—are gaining attention. Pilot studies, including those involving the Virta Health program, suggest that combining lifestyle interventions with medication tapering can maintain weight loss.
Patients like Lily from Michigan exemplify ongoing challenges; after losing nearly 80 pounds on Wegovy, she had to stop due to insurance changes and has since regained 20 pounds. She advocates for continued access to the drugs, viewing them as a safer and more effective solution in the long term.
The evolving landscape raises important questions about sustainable weight management strategies and the role of insurance coverage in supporting long-term health outcomes. As research progresses and policies adapt, the focus remains on balancing cost, efficacy, and patient wellbeing.
Source: https://medicalxpress.com/news/2025-09-struggle-glp-drug-wean-patients.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
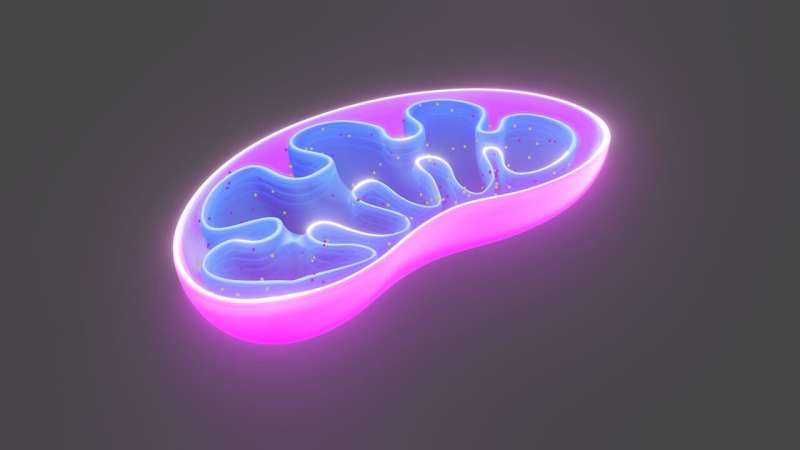
Important Discovery of Cellular Energy Regulator Could Lead to Parkinson's Disease Treatments
A new cellular switch regulating mitochondrial health has been discovered, offering promising new targets for Parkinson's disease and mitochondrial disorder treatments. Researchers highlight how modulating B55 activity could improve neuron survival and disease outcomes.
Recovery Outcomes for Older Patients After Mechanical Ventilation Are Influenced by Care Needs
This study explores how care needs influence recovery outcomes in older adults after mechanical ventilation, highlighting key factors for prognosis and long-term care planning.
Benefits of Early Aspirin Discontinuation in Low-Risk Heart Attack Patients
Research shows that early discontinuation of aspirin after MI in low-risk patients can reduce bleeding risk without increasing adverse events, thanks to advancements in revascularization techniques.
New Human Challenge Trial in Melbourne Seeks to Accelerate Strep A Vaccine Development
A human challenge trial in Melbourne is set to accelerate the development of a vaccine against Streptococcus A, addressing a major global health threat with millions affected annually.