Innovative Approach to Stem Cell Transplant Significantly Improves Outcomes for Blood Cancer Patients
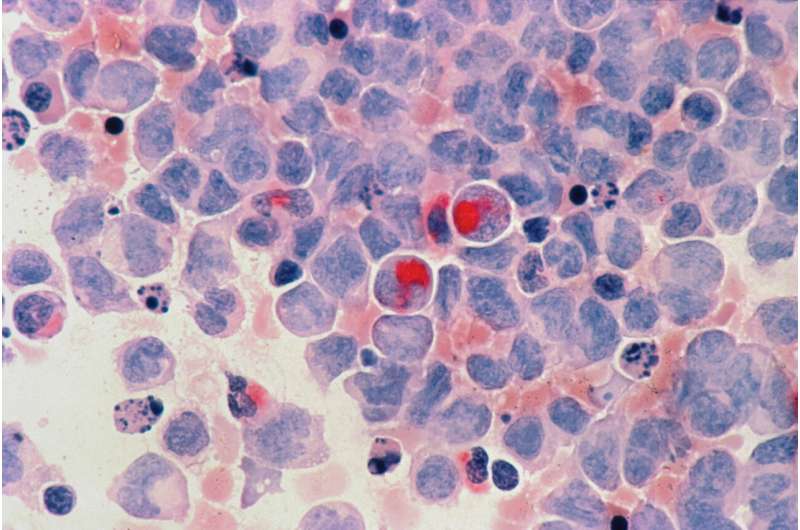
A groundbreaking Australian study introduces a new drug combination post-stem cell transplant that triples survival rates and significantly reduces GVHD risk in blood cancer patients, revolutionizing treatment standards.
Australian researchers have developed a new, less toxic drug combination that, when used after stem cell transplants for leukemia, dramatically enhances patient recovery and reduces serious complications. This breakthrough addresses critical issues such as graft-versus-host disease (GVHD), a life-threatening and often lifelong complication that can follow transplantation.
The collaborative trial, led by Monash University and the Australasian Leukemia & Lymphoma Group, has the potential to revolutionize treatments for high-risk blood cancers like leukemia. According to lead researcher Professor David Curtis, the new regimen can triple survival chances and improve quality of life three years post-transplant. Importantly, it also reduces the incidence of GVHD, which currently affects 20% of transplant patients and contributes to death or chronic health issues.
Blood stem cell transplants are vital for treating leukemia, especially for aggressive cases. However, their success has been hampered by complications such as infections, organ damage, and GVHD, which results from donor immune cells attacking the recipient's tissues. The standard method for preventing GVHD has remained unchanged for over four decades.
The recent trial evaluated 134 patients aged 18-70 across eight sites in Australia and New Zealand. It compared the traditional drug combination with a novel regimen involving cyclophosphamide and cyclosporin. Results showed a significant increase—from 14.2% to 49.1%—in patients who were alive, in remission, and free of GVHD after three years. Additionally, the occurrence of severe side effects dropped from 32.4% to 19.7% with the new approach.
These promising findings, published in the New England Journal of Medicine and presented at EHA 2025 in Milan, suggest that this simplified and safer treatment protocol could become the new standard of care for patients receiving stem cell transplants from matched siblings. The improved outcomes and reduced toxicity mark a significant step forward in blood cancer treatment therapies.
For more details, see: source
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Nasal Sprays as a Potential Needle-Free Alternative for Emergency Adrenaline Delivery in Anaphylactic Reactions
Emerging research suggests nasal sprays may replace injections for delivering adrenaline during severe allergic reactions, offering a quicker, needle-free, and portable solution for managing anaphylaxis in emergency situations.
Innovative At-Home Diagnostic Test Enhances Detection of COVID-19 and Cancer with Unprecedented Accuracy
A new at-home biosensing technology utilizing the coffee-ring effect, plasmonic nanoparticles, and AI offers rapid and highly sensitive detection of COVID-19 and cancer biomarkers, paving the way for accessible disease diagnostics.
Newer Antiseizure Medications During Pregnancy May Pose Less Risk Than Older Drugs
Recent research indicates that certain newer antiseizure medications may pose fewer risks of birth defects during pregnancy compared to older drugs, guiding safer treatment choices for expectant mothers.
Medetomidine in Illicit Drugs: A Growing Concern in Opioid Overdose Cases
Medetomidine, a veterinary sedative, is increasingly being found in street drugs like fentanyl, heightening overdose risks. Learn about its emergence, dangers, and implications for public health.



