Innovative Cancer Drug Enhances Chemotherapy Response, Even in Resistant Tumors

A new oral cancer drug developed by King's College London aims to enhance chemotherapy effectiveness, even against resistant tumors, by targeting immune-suppressing proteins produced by tumor-associated macrophages. Early studies show promising results that could lead to improved cancer treatment options.
A groundbreaking study from King's College London has unveiled a new cancer drug capable of boosting the effectiveness of chemotherapy, even in tumors that have developed resistance to treatment. The drug functions by targeting a protein called heme oxygenase-1 (HO-1), produced by macrophages—immune cells that often form a barrier around tumors, hindering immune attack and reducing chemotherapy efficacy. In preclinical models, specifically mouse studies, the administration of KCL-HO-1i, an oral inhibitor of HO-1, successfully disarmed this immune shield, allowing chemotherapy drugs to work more effectively. This is particularly promising because the drug can be taken orally at home, making it more convenient and less burdensome for patients.
The research highlights that tumors often manipulate the immune system to evade treatment. Macrophages in the tumor microenvironment release HO-1, which protects the tumor and impairs beneficial immune responses. By inhibiting this enzyme, the new drug helps restore the immune system’s ability to combat cancer and enhances the response to standard chemotherapy. The scientists have already observed positive results across various chemotherapy regimens in early laboratory tests, especially against breast cancer models.
Looking ahead, the researchers plan to initiate clinical trials within the next two years to evaluate the safety and effectiveness of KCL-HO-1i in humans. This approach could potentially be used across multiple cancer types, broadening the scope of existing treatments. Experts involved in the study emphasize that this combination strategy might not only improve patient outcomes but also reduce the need for more aggressive treatments in the future.
The development of this drug represents a significant step forward in understanding how tumors evade immune defenses and how to counteract these mechanisms to improve cancer therapy outcomes. The multidisciplinary team, which includes Professors James Arnold, James Spicer, and Miraz Rahman, underscores the importance of targeting tumor-assisted immune suppression as part of comprehensive cancer treatment strategies.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
The Impact of Skin-to-Skin Contact on Brain Development in Preterm Infants
Skin-to-skin contact, or kangaroo care, is linked to improved brain development in preterm infants, supporting emotional and cognitive growth during early hospitalization.
Potential Impact of Caffeine on Blood Transfusion Effectiveness
New research reveals that caffeine consumption by blood donors can impair red blood cell quality, potentially reducing the effectiveness of blood transfusions. The study highlights the importance of personalized transfusion strategies considering lifestyle factors and genetic traits.
WHO Reports High Mortality Rate in Recent Ebola Outbreak in Congo
The WHO reports a high mortality rate in Congo's Ebola outbreak, with 31 out of 38 cases resulting in death. Rapid spread and vaccination efforts are ongoing to control the virus.
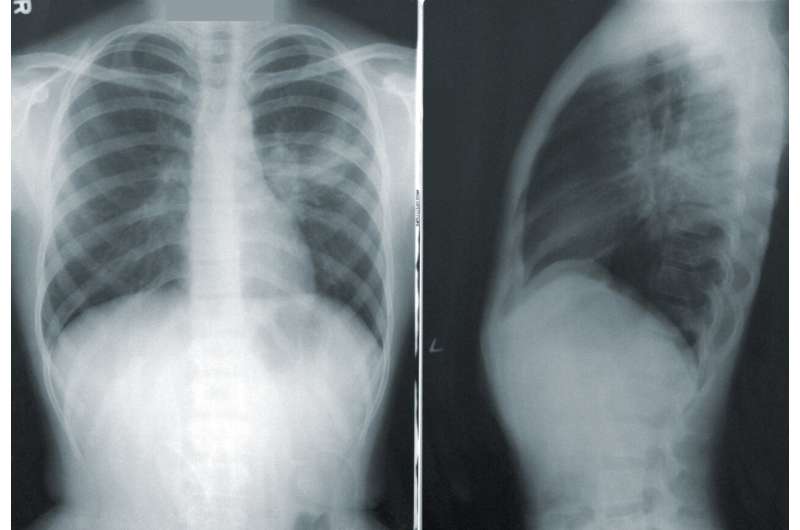
Promising Results in EGFR-Mutated Lung Cancer with Iza-bren and Osimertinib Combination Therapy
A new study demonstrates that combining iza-bren with osimertinib yields a 100% response rate in patients with EGFR-mutated non-small cell lung cancer, offering hope for improved first-line treatment options.