Researchers Identify Inflammatory Subtype of Major Depression to Enable Precision Psychiatry

Emory University researchers identify an inflammatory subtype of major depression, paving the way for personalized treatments and improved diagnostic strategies in psychiatry.
Recent research conducted by scientists at Emory University presents compelling evidence supporting the existence of an inflammatory subtype of major depression, offering new avenues for diagnosis and treatment. Led by Dr. Andrew H. Miller, a pioneer in the intersection of inflammation and depression, the study highlights inflammation as a significant factor driving depressive symptoms in approximately 25% to 30% of patients with major depression. This breakthrough is detailed across three key publications.
Dr. Miller emphasizes that understanding inflammation’s role creates an unprecedented opportunity for targeted therapies and personalized treatment strategies. His team’s research identifies biomarkers such as C-reactive protein (CRP), tumor necrosis factor (TNF), and interleukin-6 (IL-6) elevated in the blood, brain tissue, and cerebrospinal fluid of affected individuals. These markers correlate with specific symptoms, including anhedonia, fatigue, and psychomotor slowing—collectively known as "sickness behavior."
Importantly, patients exhibiting this inflammatory profile respond differently to treatments. Traditional antidepressants like selective serotonin reuptake inhibitors (SSRIs) may be less effective in this subgroup, while alternative therapies such as ketamine or electroconvulsive therapy may yield better results. This understanding underscores the importance of integrating biomarker testing into clinical practice to tailor treatments effectively.
The team advocates for including an inflammation specifier in future diagnostic manuals like DSM-6, to refine depression classification and treatment protocols. According to Dr. Miller, this could enhance clinical understanding, leading to more personalized and effective care, and accelerate research into inflammation-targeted therapies.
The recent publications—covering proposals for diagnostic updates and clinical trial designs—are published in prominent journals including JAMA Psychiatry, Biological Psychiatry, and the American Journal of Psychiatry. These works collectively advocate for the recognition of inflammation as a core component in a subset of depression, aiming to improve outcomes for millions worldwide.
This research marks a significant step toward precision psychiatry, where biological markers inform personalized treatment plans, ultimately transforming how depression is diagnosed and managed.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Climate Change Drives Increase in Rat Lungworm Disease Cases in Eastern Australia
Climate change and increased rainfall are driving a rise in rat lungworm disease in eastern Australia, affecting both animals and humans. Recent studies highlight the connection between weather patterns and disease spread, emphasizing the importance of monitoring environmental factors to prevent outbreaks.
Probiotics: Their Role in Gut Recovery Post-Antibiotics Is Complex
Research reveals that the effects of probiotics on gut recovery after antibiotics are strain-specific and complex, highlighting the need for personalized microbiome therapies.
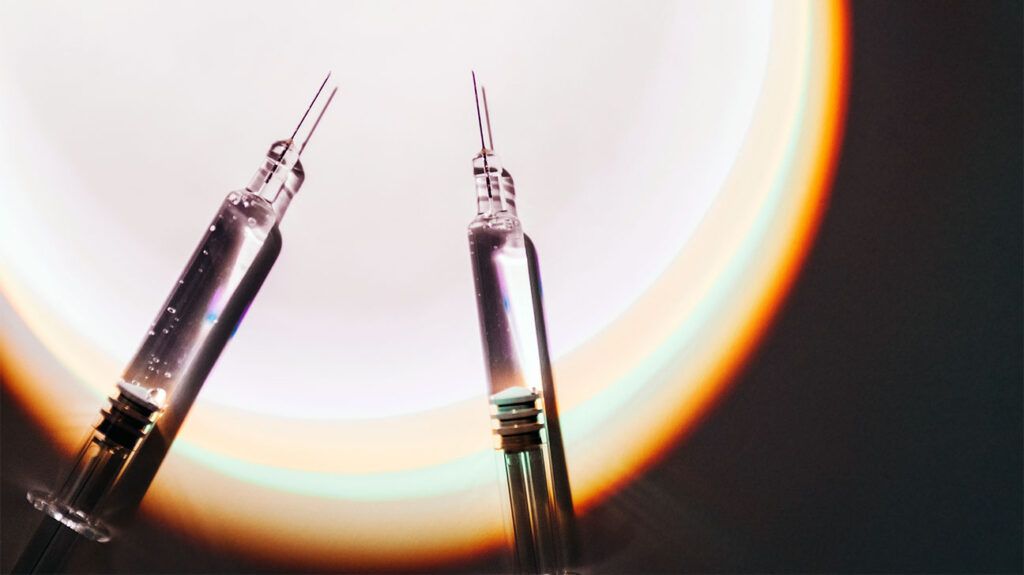
Experimental Injectable Drug Shows Promise in Treating Aggressive Breast and Skin Cancers
A new injectable immunotherapy drug shows promising results in shrinking aggressive breast and skin cancer tumors, marking a significant step forward in cancer treatment research.
Aging Reduces Overactive Immune Genes, Leading to Improvement in Lupus Symptoms in Older Adults
Aging appears to diminish the activity of immune-related genes in lupus patients, potentially leading to symptom improvement in older adults. This discovery opens new possibilities for age-specific treatments and understanding disease progression.