The Importance of Numerical Communication in Medical Risk Assessment

Effective medical risk communication involves using clear, scientific numbers to help patients accurately understand health threats, improving decision-making and trust.
When healthcare providers describe procedures or health risks without including specific numerical data, patients may misjudge the actual level of danger involved. Terms like "rarely risky" or "common side effect" can be vague and subjective, leading to overestimations or underestimations of health threats. Recent research emphasizes the importance of using concrete numbers when communicating medical risks to improve patient understanding and decision-making.
A study published in the Journal of General Internal Medicine on April 29 highlights that patients often overestimate risks when only verbal descriptors are used. For example, saying "headache is a common side effect" might not effectively convey how likely it is compared to giving a specific percentage, such as "7% of people experience headaches." Experts recommend that physicians incorporate clear, scientifically-backed numerical information to assist patients in making better-informed health choices.
According to Ellen Peters, a psychology professor at the University of Oregon, including numbers in risk communication helps demystify medical data and enhances trustworthiness. Her research shows that patients tend to feel more confident and perceive doctors as more credible when numerical data accompanies verbal advice. These findings are backed by recommendations from physicians Paul K.J. Han and Clara N. Lee, who advocate for strategies that improve shared decision-making.
Effective communication involves several key strategies:
- Using numeric data alongside verbal descriptions to clarify probabilities, e.g., "there is a 7% chance of headache, a common side effect."
- Simplifying complex medical information to avoid cognitive overload, focusing on the most relevant facts.
- Framing statistical data with contextual labels, like comparing survival rates of different treatments.
- Acknowledging uncertainty in risk estimates to set realistic expectations.
- Employing teach-back methods where patients explain in their own words what they understood, ensuring clarity.
Use of these techniques can bridge gaps in health literacy and help patients better understand their health risks. They facilitate more informed choices, foster trust in healthcare providers, and support effective shared decision-making. Given the limited time during medical appointments, clinicians can adopt quick, scripted methods to communicate complex data efficiently.
Ultimately, making numbers an integral part of health discussions can prevent patients from over- or underestimating risks, leading to more accurate perceptions and healthier outcomes.
source: https://medicalxpress.com/news/2025-05-doctors-patients-misjudge-health.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
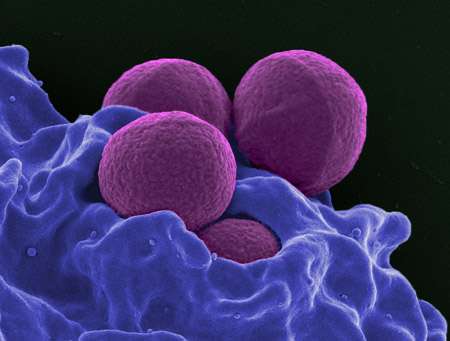
WHO Calls for Accelerated Action Against Drug-Resistant Superbugs
The WHO warns that the global pipeline for new antibiotics and diagnostics is dangerously limited, risking a surge in drug-resistant infections worldwide. Urgent investment and innovation are needed to combat antimicrobial resistance effectively.
New Insights into Prefrontal Brain Pathways: Separating Motivation from Threat Response
New research uncovers how specific prefrontal pathways regulate motivation and threat responses, offering insights into treatments for depression and anxiety.
Innovative Intergenerational Care: Connecting Young and Older Adults in Purpose-Built Communities
A groundbreaking intergenerational living model in South Australia connects seniors and children, promoting well-being, empathy, and community through purpose-built shared spaces and activities.