Impact of Symptom Dismissal by Healthcare Professionals on Patient Well-Being

A Rutgers Health review highlights how dismissing patient symptoms can cause lasting psychological and health-related harm, urging healthcare providers to validate experiences and improve communication.
When healthcare providers dismiss or minimize patients' symptoms, it can lead to significant psychological and physical consequences, a phenomenon often referred to as "symptom invalidation" or "medical gaslighting." A comprehensive review conducted by Rutgers Health researchers analyzed 151 qualitative studies involving over 11,000 individuals suffering from conditions such as fibromyalgia, long COVID, endometriosis, and lupus, all of which are challenging to diagnose. The findings reveal that patients frequently question their own reality, asking whether their symptoms are imaginary or mentally fabricated. These experiences can foster feelings of self-doubt, shame, and fear, which may escalate into depression, anxiety, or even trauma-related responses.
The research categorizes the harm caused by invalidation into four main areas: emotional distress like shame, deterioration of trust in healthcare providers, behavioral responses such as avoiding medical care, and diagnostic delays that can worsen health outcomes. Many patients report downplaying their symptoms to avoid seeming overly dramatic or to prevent confrontation with clinicians, leading some to entirely avoid seeking medical assistance even for unrelated health issues.
This trend is particularly prominent in encounters where a clear diagnosis cannot be established, a situation increasingly common with complex conditions like long COVID and postural orthostatic tachycardia syndrome. Experts attribute the prevalence of symptom invalidation to gaps in medical training, which often emphasize algorithm-driven procedures over nuanced listening, especially in uncertain cases.
To address this, the authors recommend that healthcare providers validate patient experiences regardless of immediate diagnostic clarity. Transparency about diagnostic uncertainty and avoiding reassurance that symptoms are “probably nothing serious” can foster trust and reduce distress. For patients, self-advocacy—such as researching clinicians' reputations and bringing support persons to appointments—may help, though these strategies can be demanding.
Overall, the study underscores the urgent need for medical professionals to acknowledge patients' symptoms sincerely and to foster open, empathetic communication. Doing so can mitigate psychological harm, promote faster diagnosis, and improve health outcomes. Future interventions should focus on preventing symptom invalidation to enhance both mental health and physical well-being.
Source: https://medicalxpress.com/news/2025-05-doctors-dismiss-symptoms-patients.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Fatty Liver During Pregnancy May Elevate Risk of Preterm Birth
Pregnant women with fatty liver disease face a significantly higher risk of preterm birth, highlighting the need for careful monitoring and management during pregnancy.
Innovative Bioengineered Hydrogel Extends Preservation of Live Tumor Tissues for Advanced Cancer Research
A novel bioengineered hydrogel mimicking the tumor environment has been developed to preserve live cancer tissues longer, enhancing drug testing and personalized treatment strategies for challenging cancers like peritoneal metastases.
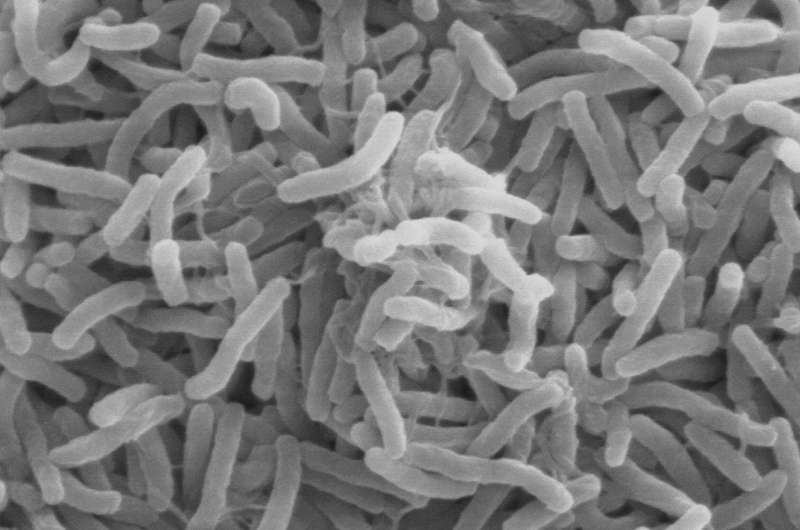
Cholera Outbreak Reported in Ivory Coast with Seven Fatalities
Ivory Coast has confirmed a cholera outbreak near Abidjan, with seven deaths and over 45 cases reported, highlighting ongoing sanitation challenges and global health risks.