Could HPV Be a Hidden Cause of Skin Cancer?
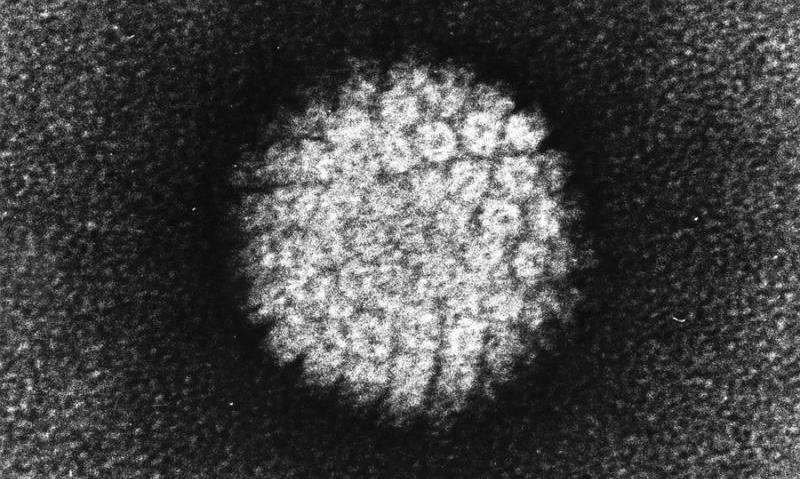
Emerging evidence suggests that human papillomavirus (HPV) may contribute to certain skin cancers, especially in individuals with immune deficiencies, expanding our understanding of skin cancer causes beyond UV radiation.
Skin cancer is predominantly linked to damage caused by ultraviolet (UV) radiation from sun exposure, which leads to mutations in skin cells. However, a recent groundbreaking case study has revealed that human papillomavirus (HPV) might also play a role in the development of certain skin cancers. Published in the New England Journal of Medicine, this report focuses on a 34-year-old woman who suffered from recurrent squamous cell carcinomas (SCC), the second most common form of skin cancer.
This patient exhibited multiple wart-like growths on her skin and inside her mouth. These growths were linked to an HPV infection. While HPV is widely recognized for causing genital warts and its association with cervical cancer, only a handful of HPV types have been proven to cause cancer. Known carcinogenic strains include HPV 16 and 18, but in this unique case, scientists identified a less-studied strain, HPV19, as a driver of the tumor.
The woman's medical history included several unsuccessful surgeries and immunotherapy treatments aimed at removing the persistent SCCs on her forehead. Her healthcare team suspected an underlying immune deficiency affecting her body's ability to combat tumors. To investigate further, scientists analyzed her tumor tissue genetically. Typically, skin cancers caused by UV exposure show a distinct set of mutations. Intriguingly, her tumor lacked these UV-related mutations. Instead, the genetic analysis revealed integration of HPV DNA into her tumor’s genetic material, indicating that the virus was directly contributing to her cancer's growth.
This case is particularly remarkable because HPV19 had not previously been linked to skin cancer. It exemplifies how, under certain immune conditions, other HPV types can initiate carcinogenesis. Her condition stemmed from inherited mutations impairing her immune responses—specifically, in the ZAP70 gene, which affects T-cell function, and RNF168, involved in DNA repair. Her compromised immune system was insufficient in detecting and eliminating HPV-infected cells.
Remarkably, after receiving a stem cell transplant that replaced her faulty immune cells with healthy ones, the woman’s immune system regained its ability to identify and destroy HPV-infected cells. This intervention led to her complete recovery and a significant reduction in tumor recurrence risk.
This case underscores the critical role of immune health in preventing cancer. It also highlights how advancements in genetic sequencing enable personalized cancer diagnosis and treatment. The findings suggest that clinicians should consider screening for HPV infections in patients with aggressive, recurrent skin cancers, especially those with immune deficiencies. These insights open potential new avenues for immunotherapy and preventive strategies against skin cancers driven by viral infections.
Overall, this case broadens our understanding of skin cancer etiology beyond UV damage, pointing to the significance of viral and immune interactions. Further research is essential to determine the prevalence of HPV-associated skin cancers and to develop targeted therapies that enhance immune surveillance.
Source: https://medicalxpress.com/news/2025-08-skin-cancer-hpv-potential.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Single Dose of Antibiotic as Effective as Multiple Doses for Treating Early Syphilis, Study Finds
A new clinical trial reveals that a single injection of benzathine penicillin G is as effective as multiple doses for treating early syphilis, offering a simpler treatment option and potentially improving patient adherence.
Exploring Botox as a Potential Treatment for Jaw Pain in TMJ Disorder
Recent research highlights the potential of Botox injections directly into the TMJ as a safe and effective treatment for jaw pain caused by TMD, offering hope for improved management of this debilitating condition.
Senate Report Reveals 31% Reduction in U.S. Cancer Research Funding Under Trump Administration
A Senate report reveals a 31% reduction in U.S. cancer research funding during the first quarter of 2025 under the Trump administration, impacting grants, staff, and public health data, raising concerns over scientific progress.



