Research Highlights Significant Health Insurance Gaps Among Adopted Children in the U.S.

A recent study reveals significant disparities in health insurance coverage among adopted children in the U.S., particularly affecting international adoptees and children of non-citizen adoptive parents. Understanding these gaps is crucial for targeted policy reforms to ensure equitable healthcare access.
Every year, hundreds of thousands of children are adopted across the United States, yet many of these children face gaps in health insurance coverage following their adoption. A comprehensive study conducted by the University of Maryland School of Public Health, published in the journal Health Affairs, sheds light on how insurance coverage varies markedly depending on factors such as the type of adoption—domestic or international—and the citizenship status of the adoptive parent.
The research highlights that adopted children often have diverse and complex health needs, including physical and cognitive challenges. Previous studies suggested that most adopted children were insured, but this new investigation reveals a more nuanced picture. The study found a particularly alarming uninsured rate of 30.7% among internationally adopted children brought into the U.S. by non-citizens. In contrast, children adopted domestically or by U.S. citizens generally have higher coverage rates.
A key focus of the study was on four specific groups: domestic adoptees, international adoptees by U.S. citizens, international adoptees by non-U.S. citizens, and children living with relatives other than their biological parents, such as grandparents. Notably, children adopted internationally by non-U.S. citizens face the highest uninsured rates, alongside lower participation in private and public health insurance programs. These adoptive parents are often more likely to share the same race as the child, have incomes below the federal poverty line, and less homeownership compared to other groups.
The researchers analyzed data from the American Community Survey spanning 2018 to 2022, involving over three million children. Findings indicate that children living with relatives other than their biological parents also have elevated uninsured rates, around 7.3%. Conversely, children adopted domestically or by U.S. citizens are more likely to have private health insurance, with rates of 56.2% and 89.1%, respectively. Interestingly, international adoptees of U.S. citizens are often better insured than nonadopted children.
The study emphasizes that adopted children cannot be viewed as a homogeneous group, as demographic and legal differences significantly impact their access to healthcare. Policy adjustments are essential to address these disparities and ensure all adopted children receive appropriate health coverage. The authors underscore the need for tailored policy interventions to reduce insurance gaps among vulnerable adoptee populations.
Source: Medical Xpress
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Innovative Use of AI and Historical Imaging Provides New Perspectives on Head and Neck Cancers
Exploring how AI and historical imaging techniques are revolutionizing the understanding and treatment of head and neck cancers through comprehensive data integration and analysis.
Rifampin Shows 99.9% Effectiveness Against Typhoid Fever
Discover how rifampin, a widely used antibiotic, is showing remarkable promise with 99.9% effectiveness against typhoid fever by removing bacterial protective capsules, offering new hope in fighting resistant strains.
Understanding the Connection Between Diabetes and Dementia
Recent research highlights the strong link between diabetes and dementia, emphasizing how blood sugar management can help preserve cognitive health and prevent decline.
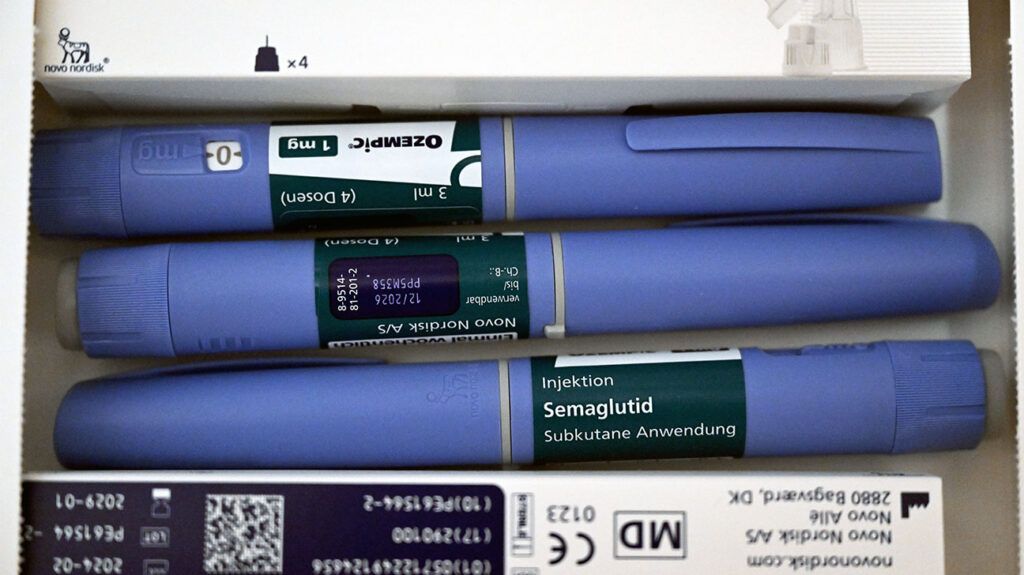
Potential Benefits of GLP-1 Drugs for Asthma Control in Obese Patients
New research suggests GLP-1 medications, used for diabetes and weight loss, may also improve asthma control in obese individuals. Learn about the promising findings and potential implications for respiratory health.