Geroscience: A New Approach to Aging and Chronic Disease Prevention

Geroscience introduces innovative strategies to slow aging and delay chronic diseases, aiming to extend healthspan and transform healthcare for an aging population.
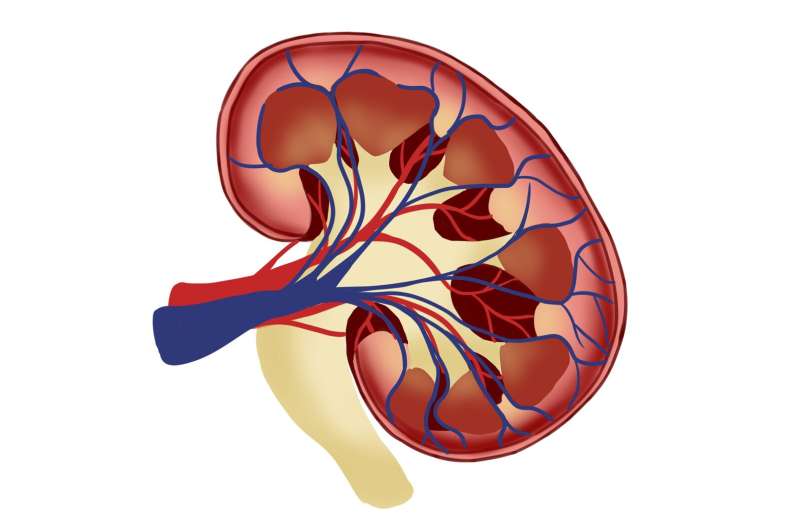
Geroscience is an emerging field that aims to transform how medicine addresses aging by focusing on the biological processes underlying age-related decline. A recent review published in JAMA highlights innovative strategies to slow biological aging, which could significantly prevent or delay multiple chronic diseases simultaneously, presenting a promising shift in modern healthcare. The concept encourages moving away from treating individual diseases like heart disease, cancer, or kidney disease in isolation, and instead targeting the root biological mechanisms that drive aging.
This approach, termed geroscience, emphasizes the importance of extending 'healthspan'—the years lived in good health free from disability and disease—by modifying fundamental pathways of aging. With the aging population in the U.S. expected to rise by over 30 million adults over 65 by 2050, healthcare systems face the risk of being overwhelmed if current disease-by-disease treatment methods persist. Geroscience offers a proactive alternative by potentially extending healthy years and reducing healthcare burdens.
A key aspect involves assessing biological age, not just chronological age, through indicators such as epigenetics. Researchers at Sutter Health’s San Francisco Coordinating Center, led by Dr. Brian Chen, are exploring whether biological age better predicts health outcomes like hospitalizations compared to traditional age measures. Their work aims to tailor treatments based on an individual’s biological aging process.
Current research is also investigating existing therapies for their potential to slow the aging process. These include metformin, a longstanding diabetes medication with possible anti-aging effects; GLP-1 receptor agonists like semaglutide, used for diabetes and obesity, which might mimic calorie restriction benefits; and senolytics, drugs designed to target and eliminate senescent cells that contribute to inflammation and tissue deterioration. While none of these therapies are yet approved by the FDA explicitly for anti-aging, ongoing clinical trials may pave the way for future standards of care aimed at preserving overall function and independence.
Dr. Cummings emphasizes that understanding and modulating these pathways could potentially slow aging and promote longer, healthier lifespans, both for Sutter patients and worldwide. As geroscience advances, it holds the promise of a paradigm shift in medicine—transforming aging from an inevitable decline to a manageable biological process that can be influenced to enhance quality of life.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Breakthrough in Treating Rare Kidney Disease C3G with Targeted Therapy
A groundbreaking treatment for the rare kidney disease C3G has been developed, targeting its underlying immune cause. Clinical trials show promising results in preventing kidney damage and disease progression. Learn more about this medical breakthrough.
Electronically Connected Lung Cancer Cells in the Brain Promote Tumor Growth
Scientists have revealed that small cell lung cancer cells in the brain can form electrical synapses with neurons, promoting tumor growth. Disrupting neural signaling may offer new therapeutic possibilities for brain metastases.
Innovative Brain Organoid Platform Aims to Elucidate Repeated Low-Level Blast Injuries in Military Brain Trauma Research
A pioneering brain organoid platform developed by Johns Hopkins researchers aims to unlock the mysteries of repeated low-level blast injuries in military personnel, advancing TBI research and prevention strategies.