Genetic Factors and Anticoagulant Use Associated with Increased Intracranial Hemorrhage Risk in Atrial Fibrillation Patients
New research links the APOE e4 genetic allele and Eliquis use to increased risk of intracranial hemorrhage in atrial fibrillation patients, highlighting potential for personalized treatment strategies.
A recent study published in JAMA Neurology has revealed a connection between genetics, anticoagulant therapy, and the risk of bleeding within the skull among patients with atrial fibrillation. Researchers found that individuals carrying the APOE e4 genetic allele who are treated with Eliquis (apixaban), a common blood thinner, face a higher likelihood of experiencing intracranial hemorrhage compared to those without this genetic marker.
This research was spearheaded by Santiago Clocchiatti-Tuozzo, MD, MHS, from Yale School of Medicine, as part of his postdoctoral fellowship. The team focused on understanding how the APOE e4 allele, known for its role in Alzheimer’s disease, influences bleeding risk in anticoagulated patients. Given the established link between this allele and intracranial hemorrhage in patients using older anticoagulants like warfarin (Coumadin), the study extended its investigation to newer drugs like Eliquis, which are prescribed to prevent strokes triggered by atrial fibrillation.
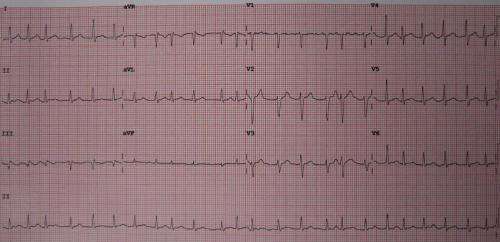
Atrial fibrillation causes irregular heart rhythms, increasing the risk of clot formation that can lead to ischemic strokes. Eliquis is used to reduce this risk by thinning the blood, but this study indicates that genetic factors such as APOE e4 may complicate treatment outcomes. Although intracranial hemorrhage is a rare side effect, it remains one of the most feared complications associated with anticoagulant therapy.
The study outcomes suggest that genetic testing for APOE e4 could help personalize treatment strategies, potentially identifying patients at higher risk for severe bleeding events. This insight not only enhances understanding of bleeding risks associated with anticoagulants but also holds implications for broader neurological conditions, including Alzheimer’s disease, given the genetic overlap.
Future research aims to incorporate neuroimaging techniques and explore other genetic contributors to both intracranial hemorrhage and ischemic stroke in atrial fibrillation patients on anticoagulants. Such advancements could lead to more precise and individualized preventative measures, improving patient safety and outcomes.
The findings emphasize the importance of considering genetic profiles when prescribing anticoagulants, paving the way for personalized medicine approaches in managing stroke and bleeding risks.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Effective Strategies for Communicating with Loved Ones About a Head and Neck Cancer Diagnosis
Learn effective strategies to communicate openly and supportively with loved ones after a head and neck cancer diagnosis. Practical tips include understanding your diagnosis, deciding who to inform, and seeking support resources to navigate this challenging time.
Enhancing Hospital Discharge Summaries: A Call for Tailored Communication
A new study highlights the need for personalized and purpose-driven hospital discharge summaries to improve patient care and enhance communication between hospitals and GPs. Experts emphasize understanding GP perspectives for better discharge communication.
Innovative Safety Device Extends Survival Time During Avalanches by Fivefold
A new safety device for avalanche victims has been shown to increase survival time fivefold by delivering oxygen directly under snow, providing crucial extra minutes for rescue operations.
Innovative Algae-Based Gel Enhances Breast Cancer Research Capabilities
A groundbreaking algae-derived hydrogel developed by UCSB researchers offers a customizable platform for studying breast tissue development and cancer progression, with potential applications in regenerative medicine.



