Genetic Mutation Influences Iron Deficiency in Crohn's Disease Patients
A groundbreaking study reveals how genetic mutations in PTPN2 impair iron absorption, leading to anemia in Crohn's disease patients, paving the way for personalized therapies.
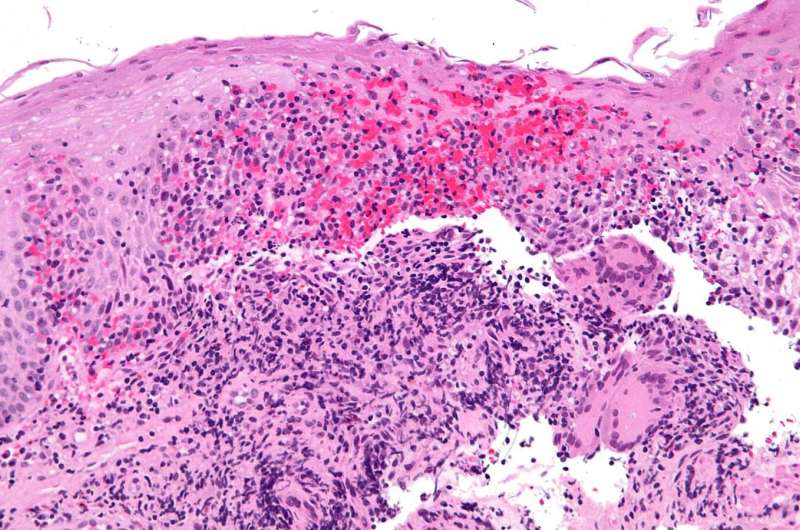
Recent research from the University of California, Riverside School of Medicine has uncovered a significant link between a genetic mutation and the severity of iron deficiency in individuals with Crohn's disease, a common form of inflammatory bowel disease (IBD). This discovery sheds light on why some patients experience persistent anemia despite receiving standard iron supplementation.
The study focused on a loss-of-function mutation in the PTPN2 gene, which plays a crucial role in regulating iron levels in the body. Researchers analyzed serum samples from IBD patients and found that carriers of this mutation, present in approximately 14-16% of the general population and 19-20% of IBD patients, exhibited disrupted iron-related blood proteins. This disruption impairs the body's ability to absorb and maintain adequate iron levels, leading to anemia.
Further experiments involving deletion of the PTPN2 gene in mice demonstrated that these animals developed anemia and showed reduced capacity to absorb iron from their diet. This was linked to decreased levels of key iron-absorbing proteins in the intestinal epithelial cells, which are responsible for nutrient uptake. The findings suggest that genetic variants like those in PTPN2 can directly interfere with iron absorption, contributing to persistent anemia in Crohn's disease patients.
"Understanding the genetic factors affecting iron handling opens new possibilities for targeted treatments," explained Dr. Declan McCole, the study’s lead author. "Patients with these genetic variants may benefit more from intravenous iron therapy instead of oral supplements, which are often ineffective in this group."
This research not only advances our understanding of the systemic complications associated with Crohn's disease but also points toward personalized treatment approaches—especially for patients resistant to conventional iron therapy. The study is published in the International Journal of Molecular Sciences and highlights the importance of considering genetic factors in managing Crohn's disease-related anemia.
Source: MedicalXpress
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
International Healthcare Workers Report on War-Related Injuries in Gaza
A recent study reveals the unprecedented severity of injuries faced by civilians in Gaza, underscoring the urgent need for robust healthcare response systems during ongoing conflicts. source: https://medicalxpress.com/news/2025-09-international-health-workers-war-injuries.html
Brain Imaging Shows Action-Based Brain Organization in Individuals Without Hands
New neuroimaging research reveals that the brain is organized around actions like tool use, rather than specific body parts, demonstrating remarkable neural plasticity even in individuals born without hands.
Artificial Intelligence Uncovers Hidden Signs of Parkinson's Disease Through Finger-Tapping Video Analysis
Cutting-edge AI technology analyzes finger-tapping videos to detect early signs of Parkinson's disease, enabling earlier diagnosis and intervention using simple video recordings.
New Insights into How a Protein Facilitates Pancreatic Cancer’s Spread to Liver and Lungs
Scientists have uncovered how the protein PCSK9 influences pancreatic cancer cells' ability to metastasize to the liver and lungs by regulating cholesterol metabolism, opening new therapeutic possibilities.



