Gene Therapy Significantly Enhances Quality of Life for Patients with Sickle Cell Disease and Beta Thalassemia
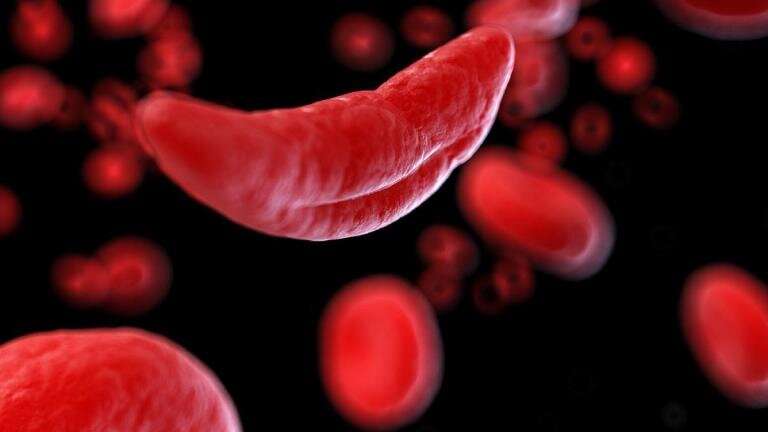
Gene therapy with exagamglogene autotemcel (exa-cel) has demonstrated remarkable and lasting improvements in quality of life for patients with sickle cell disease and beta thalassemia, offering new hope for long-term health and daily living.
Recent studies published in Blood Advances reveal that the use of exagamglogene autotemcel (exa-cel), a CRISPR-based gene therapy, has led to substantial and durable improvements in the quality of life for individuals suffering from severe sickle cell disease (SCD) and transfusion-dependent beta thalassemia. These groundbreaking findings highlight not only the clinical efficacy of exa-cel but also its profound impact on daily living, social interactions, and emotional well-being.
In the trials, patients treated with exa-cel reported meaningful enhancements across various aspects of life. These included better physical functioning, improved social and family connections, and a reduction in pain episodes. Strikingly, improvements were observed as early as six months after infusion and were sustained over long-term follow-up periods, averaging around 33 to 38 months.
Lead researcher Dr. Josu de la Fuente from Imperial College London noted, “This is the first instance where we could clearly measure improvements in quality of life following gene editing therapy. Unlike laboratory or hematologic indicators, these results demonstrate tangible benefits patients experience in their daily lives.”
The studies involved patients ranging from adolescents to adults. For sickle cell disease, quality of life scores exceeded population norms after treatment, with marked improvements in social impact (+16.5) and emotional well-being (+8.5) among adults, and significant gains in school and social functioning among adolescents. Similar positive outcomes were seen in beta thalassemia patients, where both adults and teenagers showed notable improvements in health status measured by standardized scales.
Exa-cel works by removing and editing a patient’s own blood stem cells to produce healthy hemoglobin, eliminating the need for chronic transfusions. Approved by the FDA in late 2023 for patients 12 and older, it offers a potential cure for these lifelong blood disorders. Despite its complexity and cost, experts like Dr. de la Fuente emphasize that the therapy’s benefits in restoring normal function and life quality make it a valuable treatment option.
While these findings are promising, researchers acknowledge limitations due to the reliance on patient-reported outcomes and ongoing trials. Future research aims to validate these results in larger cohorts and to further assess long-term effects.
Ultimately, exa-cel provides patients with severe hemoglobinopathies a chance at a more normal, productive life, reducing hospital visits and enabling many to return to school, work, and family activities, thus significantly transforming their overall quality of life.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
New Experimental Drug Shows Potential in Regulating Weight and Blood Sugar Levels
A new experimental drug, SANA, shows promise in stimulating fat tissue to produce heat, aiding weight loss and improving blood sugar levels, with minimal side effects. Current studies suggest it could be a breakthrough in obesity and metabolic disorder treatments.
Study Finds Very Low Reversal Rate of Legal Gender Changes in Sweden
A groundbreaking study from Uppsala University shows that less than 1% of individuals in Sweden who change their legal gender later revert, highlighting the stability of gender transitions over ten years.
Insights into the Early Stages of Lung Fibrosis Through Tissue Stiffening
New research reveals how tissue stiffening in the lungs can be a key early indicator and trigger of fibrosis, opening doors for earlier diagnosis and intervention.



