Ethnic Variations in Routine Blood Tests and Cancer Risk Prediction in Primary Care

Research shows that routine blood tests for cancer risk are less effective in Asian and Black patients compared to white patients, highlighting the need for more personalized diagnostic strategies in primary care.
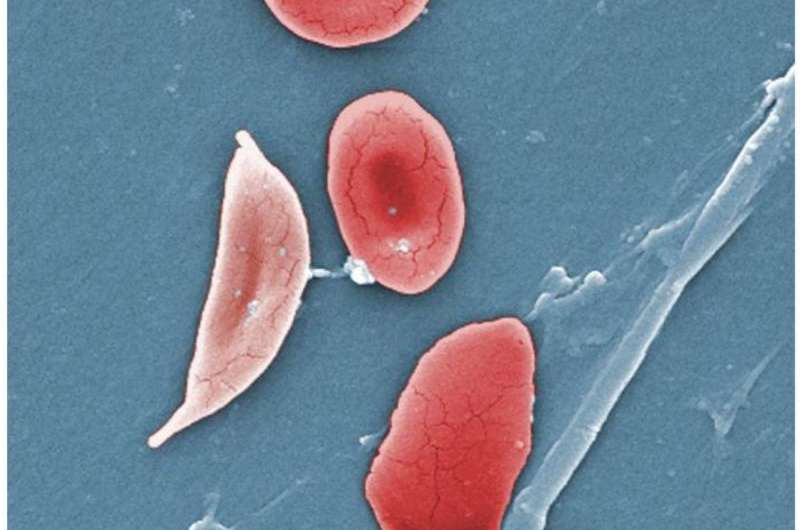
A recent study conducted by researchers at the University of Exeter has revealed significant differences in the effectiveness of routine blood tests for predicting cancer risk across different ethnic groups. The study focused on common blood markers used in primary care, such as hemoglobin levels and mean corpuscular volume (MCV), which are typically employed to assess anemia and other health conditions.
The findings indicate that while these blood tests are valuable in predicting subsequent cancer risk among white patients, their predictive power is notably weaker among Asian and Black patients. Notably, low hemoglobin and low MCV, which are often indicators of iron deficiency anemia, did not reliably signal increased cancer risk in these populations. The strongest association with cancer diagnoses, particularly colorectal and esophageal-gastric cancers, was observed in white patients.
Published in the British Journal of General Practice, this research underscores the limitations of current diagnostic guidelines that do not account for ethnic variability. Dr. Tanimola Martins, a senior research fellow involved in the study, emphasized the need for more personalized approaches. He highlighted that these disparities likely stem from a combination of biological differences, lifestyle factors, socioeconomic status, and variations in healthcare access and testing frequency.
The implications are considerable, as early detection is crucial for improving cancer survival rates. Currently, guidelines primarily consider factors like age and sex, but fail to incorporate ethnicity, despite evident differences in cancer incidence and outcomes among diverse populations. For example, while white populations may have a higher overall risk of certain cancers, Black and Asian patients are often diagnosed at more advanced stages, particularly for gastrointestinal cancers.
This study calls for further research to understand these disparities and advocates for developing diagnostic strategies that are more inclusive and tailored to different ethnic groups. By doing so, healthcare providers can ensure timely and accurate cancer investigations for all patients, ultimately reducing health inequalities.
Source: https://medicalxpress.com/news/2025-08-primary-routine-blood-cancer-differ.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Innovative Treatment Algorithms Reduce Hospitalizations for Children with Sickle Cell Disease
Implementing standardized treatment algorithms for children with sickle cell disease at MUSC has led to a significant reduction in hospital stays while maintaining patient safety and improving quality of life. Discover how this collaborative approach is shaping future pediatric care.
Nepal's Health Insurance Initiative: Challenges and Early Outcomes
A recent study evaluates Nepal's National Health Insurance Program, revealing challenges like low enrollment and administrative issues, while highlighting its potential to improve healthcare utilization with systemic improvements.
Exploring the Impact of Illusory Beliefs on Medical Behavior and Trust in Healthcare
A recent study explores how false health beliefs influence trust in medicine and the use of unproven therapies, highlighting the importance of health literacy and evidence-based decision-making.
Rising Gonorrhea Cases Highlight Challenges of Antibiotic Resistance
Gonorrhea cases are rising worldwide, fueled by increasing antibiotic resistance, making effective treatment more challenging. Researchers are working on new drugs to combat resistant strains and prevent severe health complications.