New Survey Highlights Discrepancies in How Patients with Obesity and Doctors View the Causes and Goals of Obesity

A global survey uncovers significant gaps between how people with obesity and healthcare providers perceive the causes of obesity and their treatment goals, emphasizing the need for more compassionate, evidence-based care.
A recent international survey involving adults with obesity and their healthcare providers across seven countries has revealed significant differences in perceptions regarding the causes of obesity and treatment priorities. Presented at the European Congress on Obesity (ECO25) in Malaga, Spain, the study underscores the existence of widespread misconceptions and biases that can negatively influence access to effective care.
The survey found that many physicians typically attributed their patients’ obesity primarily to behavioral factors such as overeating (69%), lack of physical activity (61%), and high-fat diets (51%). These causal attributions became more pronounced with increasing severity of obesity, with three-quarters of physicians citing overeating as the top cause in patients with class III obesity. Conversely, patients themselves recognized biological factors, including genetics, which they ranked as the third leading cause—higher than physicians did, who on average placed genetics seventh.
Lead researcher Dr. Ximena Ramos Salas emphasized that misconceptions about obesity being solely a matter of personal choice contribute to stigma and hinder comprehensive, evidence-based management. Despite obesity being classified as a chronic disease characterized by complex biological and environmental factors, healthcare systems often fall short in providing appropriate, person-centered treatment.
The survey also revealed disparities between the treatment goals of physicians and patients. While clinicians prioritized health outcomes such as improving quality of life, mobility, and blood pressure, patients' aspirations centered around psychosocial improvements like appearance, confidence, and fitting into smaller clothing sizes. Dr. Ramos Salas highlighted that healthcare providers can improve care by focusing on overall health and well-being rather than just weight loss, also addressing internalized stigma to promote body acceptance and confidence.
This comprehensive study involved analyzing 1,379 responses from patients and physicians in multiple countries, offering vital insights into the need for enhanced awareness and education to bridge perception gaps and reduce bias in obesity care.
Source: https://medicalxpress.com/news/2025-05-survey-reveals-high-disconnect-perceptions.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
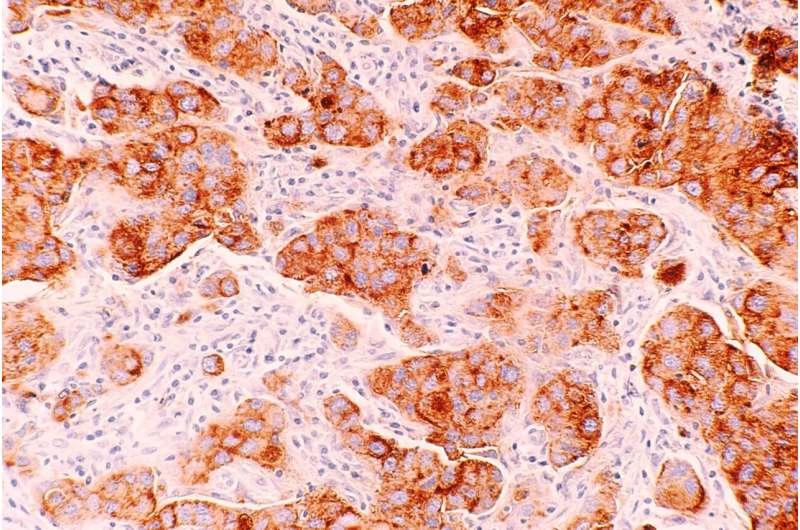
How Cell Metabolic Communication Hampers Anti-Tumor Immune Responses
New research reveals how cancer cells manipulate neighboring cells’ metabolism, promoting immune suppression and tumor growth, opening potential pathways for improved cancer therapies.
Understanding Molecular Interactions That Promote Cell Migration in Brain Cancer
New research uncovers how proteins like shootin1b regulate cell migration in glioblastoma, opening pathways for targeted cancer therapies.
Approximately 29% of Infants Receive RSV Immunization in the 2023-2024 Season
In the 2023-2024 season, nearly 30% of infants in the U.S. received RSV protection via vaccination or monoclonal antibodies, highlighting ongoing efforts to combat severe respiratory infections in newborns.