Cholesterol Drug Repurposed to Improve Blood-Brain Barrier and Neuropsychiatric Outcomes in DiGeorge Syndrome

Research reveals that cholesterol-lowering drugs may restore mitochondrial function and improve blood-brain barrier integrity, offering new hope for neuropsychiatric conditions in DiGeorge syndrome.
Recent research indicates that targeting mitochondrial dysfunction at the blood-brain barrier (BBB) could offer new therapeutic avenues for individuals with DiGeorge syndrome (22qDS), a genetic disorder associated with increased risk of neuropsychiatric conditions such as schizophrenia. A collaborative effort between the University of Pennsylvania School of Veterinary Medicine (Penn Vet) and Children's Hospital of Philadelphia (CHOP) has uncovered that mitochondrial deficits contribute to a compromised BBB, leading to neurodevelopmental challenges in 22qDS patients.
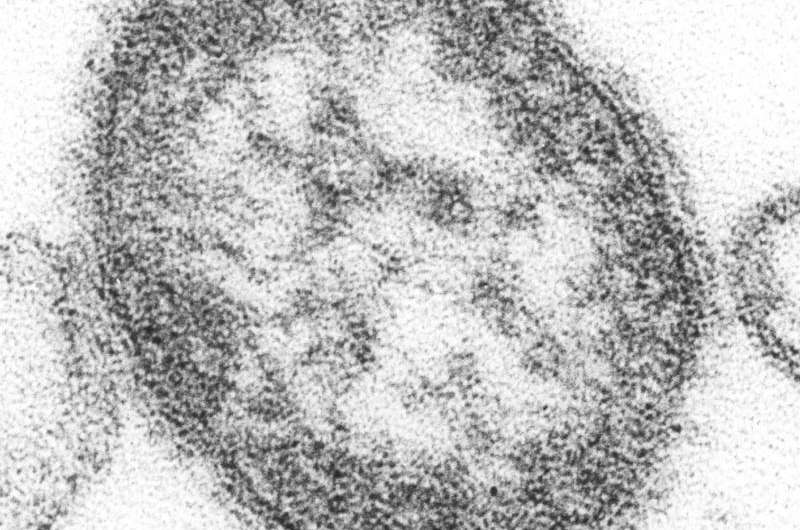
The BBB is a vital vascular structure that maintains brain homeostasis, preventing harmful substances from entering the brain while allowing essential nutrients through. Interestingly, the BBB contains a higher mitochondrial content compared to peripheral blood vessel endothelial cells, underscoring its reliance on mitochondrial health. In 22qDS, which involves the deletion of six mitochondrial genes, this mitochondrial impairment results in a 'leaky' BBB, contributing to neuropsychiatric symptoms such as psychosis. Approximately one in four individuals with 22qDS may develop schizophrenia, highlighting the urgency for targeted treatments.
The study focused on human-induced pluripotent stem cell-derived brain microvascular endothelial cells from patients with 22qDS and BBB models from preclinical studies. Findings demonstrated that mitochondrial dysfunction weakens BBB integrity, but encouragingly, treatments can restore function. The team tested bezafibrate, an FDA-approved cholesterol-lowering drug known to activate mitochondrial biogenesis and turnover. Treatment with bezafibrate improved mitochondrial health, strengthened BBB function, and corrected social memory deficits in animal models—abnormalities linked to BBB impairment and schizophrenia.
These promising results suggest that existing cholesterol drugs like bezafibrate could be repurposed to address mitochondrial and BBB dysfunction in neuropsychiatric conditions. While initial studies centered on 22qDS, researchers believe that the implications extend to other neuropsychiatric disorders involving mitochondrial pathology, including idiopathic psychosis and neurodegenerative diseases. Further clinical investigations are necessary to confirm these findings.
This groundbreaking work emphasizes the importance of mitochondrial health in maintaining BBB integrity and its impact on neuropsychiatric disorders, offering a new perspective on treatment strategies. The full research is published in Science Translational Medicine. (source: https://medicalxpress.com/news/2025-08-repurposing-cholesterol-drug-benefit-digeorge.html)
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Understanding Human Body Control and Its Implications for Parkinson's Disease Risk
Research explores how the nervous system controls human movement and how alterations in motor strategies can predict early Parkinson’s disease, offering promising avenues for early screening and intervention.
Canada Reports First Death Amid Ongoing Measles Outbreak
Canada has reported its first measles-related death amid a resurgence of the disease, primarily affecting unvaccinated communities and vulnerable groups. The outbreak has resulted in over 5,000 cases since October 2024.
Artificial Intelligence Boosts Medical Image Analysis and Radiology Efficiency
Discover how AI and visual-language models are revolutionizing medical image analysis, supporting radiologists, and enhancing diagnostic accuracy in healthcare.
Persistent Mucus Plugs Accelerate Lung Function Decline in COPD Patients
New research reveals that persistent airway mucus plugs contribute to faster lung function decline in COPD patients, highlighting potential therapeutic targets to slow disease progression.