How CAR-T Cell Therapy Is Transforming Cancer Treatment
Discover how CAR-T cell therapy is transforming cancer treatment by harnessing genetically engineered immune cells to target and destroy tumors with unprecedented precision and strength.
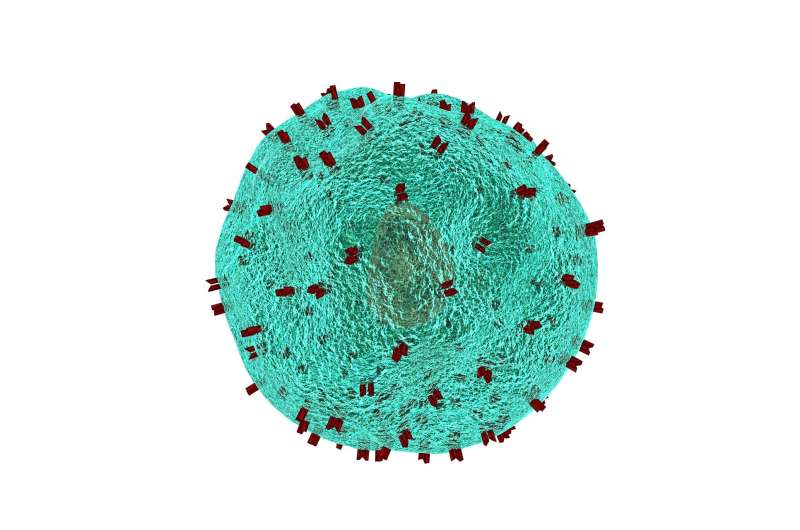
Personalized medicine has become a growing reality in modern healthcare, with CAR-T cell therapy standing out as one of its most promising innovations. This groundbreaking approach involves genetically modifying a patient's immune cells—specifically T-lymphocytes—to better recognize and attack cancer cells. The process temporarily takes cells from the patient, enhances their ability to target tumors in the lab, and then reintroduces them into the patient's body, leading to a potent immune response.
The scientific community has shown immense interest in CAR-T technology, with over 1,000 clinical trials worldwide exploring its potential, as indicated by the ClinicalTrials.gov platform. These therapies are especially effective against certain blood cancers like leukemias and multiple myelomas, where they have demonstrated remarkable success.
To understand how CAR-T cells work, it is essential to know the role of T-lymphocytes in the immune system. These cells act as the body's police force, identifying and destroying infected or abnormal cells, including cancerous ones. However, their natural ability may fall short against aggressive tumors. CAR-T cells are equipped with a next-generation receptor that functions like a highly sensitive radar, pinpointing tumor cells with incredible precision. This receptor is composed of three main parts: an external recognition domain, a signal transducer through the cell membrane, and an internal activation component that triggers an immune attack.
This engineered design makes CAR-T cells significantly more effective, producing an immune response up to 1,000 times stronger than ordinary T-cells. This enhancement allows for the destruction of cancer cells resistant to conventional therapies. Current advancements focus on refining these cells further while preventing premature exhaustion, thereby increasing their efficacy.
Despite impressive results, several obstacles remain. High costs, potential risks, and limited accessibility hinder widespread use. Although CAR-T therapy has yielded excellent outcomes in hematologic cancers, its application to solid tumors like glioblastoma or ovarian cancer presents additional challenges, such as dense tumor matrices, hostile microenvironments, and nutrient shortages that impair T-cell function.
To overcome these barriers, researchers are exploring strategies such as combining CAR-T therapy with chemotherapy, radiotherapy, or immune checkpoint inhibitors to improve tumor infiltration and efficacy. Additionally, developing 'off-the-shelf' allogeneic CAR-T cells from healthy donors could reduce costs and expand treatment access, especially when patient-derived cells are inadequate.
The future of CAR-T therapy hinges on overcoming the main hurdle: extending its benefits beyond blood cancers to solid tumors. Efforts are underway to identify tumor-specific targets like B7H3 and EGFRvIII in glioblastoma, improve delivery methods crossing the blood-brain barrier, and modulate inflammation.
Moreover, clinical investigations are expanding into alternative applications, such as treating autoimmune diseases like rheumatoid arthritis, promising broader therapeutic potential. The pharmaceutical industry is investing heavily in these therapies, with the market projected to grow exponentially from around $10.4 billion in 2024 to over $128 billion by 2032.
In summary, CAR-T cell therapy has evolved from a futuristic concept into a proven treatment for certain cancers. While challenges remain, ongoing research and technological improvements suggest that personalized immunotherapy will continue to revolutionize how we approach cancer and other immune-related conditions.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Link Between Low-Level Arsenic Exposure in Drinking Water and Adverse Birth Outcomes
New research shows that even low levels of arsenic in public drinking water may increase risks of preterm birth and low birth weight, highlighting the need for stricter water safety standards.
Lower Stroke Survival Rates in Socioeconomically Disadvantaged Areas
Research shows that people in deprived areas face higher mortality rates after stroke, highlighting the need for targeted healthcare interventions to address regional inequalities.
U.S. Government Considers Linking Tylenol to Autism Risks
The Trump administration is considering linking acetaminophen, the active ingredient in Tylenol, to autism risk and advising pregnant women to avoid its use unless necessary. This move reflects ongoing debates about medication safety during pregnancy.



