Are You Truly Allergic to Penicillin? A Pharmacist Reveals the Truth Behind Common Mislabeling
Many people are incorrectly labeled as allergic to penicillin, which can impact treatment options. Learn how testing can clarify your allergy status and improve healthcare outcomes.
Many individuals carry a penicillin allergy label, often based on childhood reactions or vague memories. However, recent research indicates that a significant portion of these labels may be incorrect. While up to 20% of Americans report being allergic to penicillin, fewer than 1% actually have a confirmed allergy. This discrepancy can impact treatment options, as inaccurately diagnosed allergies can lead to the use of broad-spectrum antibiotics, which may have more side effects and contribute to antibiotic resistance.
As a clinical pharmacy expert specializing in infectious diseases, I have seen how mislabeling can hinder the administration of optimal antibiotics. Many childhood rashes are caused by viruses or infections rather than drug allergies, yet they often get mistaken for allergic reactions. Furthermore, side effects like nausea or diarrhea are not necessarily indicators of true allergy. Interestingly, a true penicillin allergy often diminishes over time; approximately 80% of those allergic as children lose their sensitivity after about 10 years.
Understanding whether you are truly allergic involves careful assessment. Talking with a healthcare professional is essential—questions about your reactions, timing, and subsequent medication use help determine if testing is necessary. Penicillin skin testing, which involves small skin pricks and injections, is a safe method to detect true allergy. Today, in some cases, an oral challenge with small doses of penicillin or amoxicillin under supervision can confirm the absence of allergy and allow patients to safely use these antibiotics again.
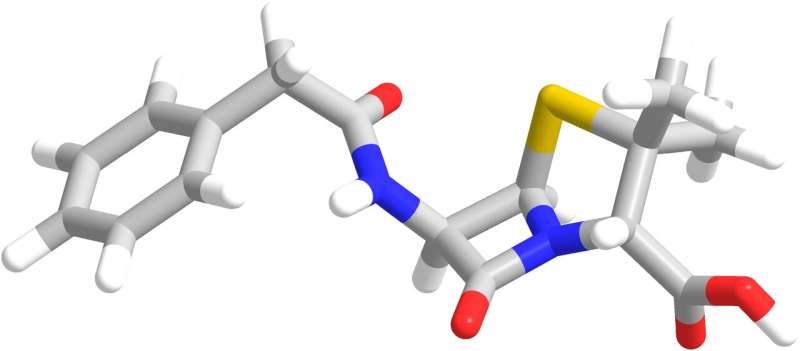
Penicillin and related antibiotics have played a crucial role in combating infections since their discovery in 1928 by Alexander Fleming. They are often the most effective choice for treating many respiratory, urinary, and dental infections. When patients are mistakenly labeled as allergic, they tend to receive alternative treatments that are less targeted, broader in spectrum, more expensive, and sometimes riskier. Correctly identifying penicillin allergies can lead to safer, more effective, and more affordable treatment options.
Mislabeling often occurs because childhood reactions are misinterpreted, or side effects are mistaken for allergies. Genetics do not play a significant role in allergy transmission, and many reported allergies are not hereditary. Most importantly, since allergies can fade over time, an outdated allergy label may no longer be accurate. Proper testing and consultation can help many people reclaim penicillin as a safe treatment choice, improving outcomes and reducing antibiotic resistance.
In conclusion, if you believe you are allergic to penicillin, it is worthwhile to seek professional assessment. Proper testing and evaluation can clarify your allergy status, potentially allowing you to receive the most effective and safest antibiotics for your infections. This not only benefits your health but also supports the global effort to combat antibiotic resistance.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Benefits of Routine Asthma Screening in High-Prevalence Communities
Implementing universal asthma screening in high-prevalence communities helps identify at-risk children early, addressing environmental triggers and improving health outcomes.
Hearing Aids and Cochlear Implants Boost Social Connection and Quality of Life
Hearing aids and cochlear implants significantly enhance social engagement and reduce isolation in adults with hearing loss, promoting better overall well-being.
Immune Cells That Clear Dead Cells May Protect Insulin-Producing Cells in the Pancreas
Scientists have identified a special type of immune cell in the pancreas that can prevent the immune attack responsible for Type 1 diabetes by silencing harmful T cells, offering new potential for disease prevention.
Rising Environmental Hazards Require Enhanced Resources for Children with Cancer
Environmental pollutants like pesticides and wildfire smoke pose serious long-term health risks for children with cancer. Experts call for better resources, policies, and support to protect vulnerable pediatric populations and improve health outcomes.



