How Air Pollution Causes Immune Imbalance and Lung Damage: New Research Insights

New research from Pusan National University reveals how long-term air pollution exposure triggers immune imbalance and lung inflammation through oxidative stress and NRF2 pathway activation, worsening respiratory conditions like asthma.
Air pollution remains a significant global health challenge, with over 90% of the world's population breathing air that surpasses safety standards set by the World Health Organization. Fine particles like PM2.5 and coarse particles like PM10 are particularly hazardous as they can penetrate deep into lung tissue and enter the bloodstream, leading to various health issues. While their connection to respiratory diseases is well documented, recent investigations reveal how these pollutants disturb immune responses within the lungs.
A groundbreaking study led by Professor Changwan Hong at Pusan National University School of Medicine in South Korea has shed light on this mechanism. The research examines how long-term exposure to particulate matter (PM10 and PM2.5) induces immune imbalance, favoring allergic-like T2 immune responses. This imbalance is mediated by oxidative stress and the activation of the NRF2 pathway, a central regulator of oxidative stress responses.
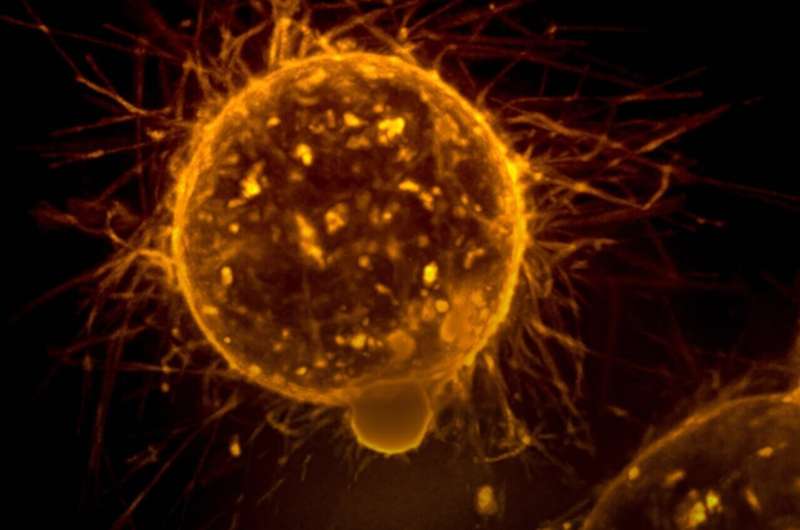
Using a mouse model, the scientists exposed mice daily to particulate matter for 16 weeks. Analyses of lung tissue, blood plasma, and immune cells revealed significant inflammation, including thickening of alveolar walls, immune cell infiltration, and tissue scarring—effects that were more pronounced with PM2.5 due to its ability to reach deeper lung areas. Notably, the immune profile shifted: protective T1 responses declined, while T2 signals, associated with allergies and asthma, increased. Elevated cytokines such as IL-4, IL-5, and IL-13 and higher levels of IgE and IgG1 antibodies indicated heightened allergic inflammation.
The link to oxidative stress is crucial. Activation of the NRF2 pathway, usually protective against environmental damage, appeared to exacerbate inflammation under chronic activation conditions. Prof. Hong explains that this mechanistic insight highlights why sustained air pollution exposure worsens conditions like asthma and allergic lung diseases, positioning NRF2 as a key driver of immune reprogramming.
This research underscores the molecular impact of pollution on respiratory health and opens avenues for therapeutic interventions targeting oxidative stress and NRF2 regulation. Modulating these pathways could potentially mitigate pollution-induced allergic inflammation. Ultimately, the findings emphasize the importance of stringent air quality regulations to safeguard vulnerable populations from long-term respiratory and immune health risks.
Source: https://medicalxpress.com/news/2025-07-air-pollution-triggers-immune-imbalance.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Groundbreaking Large-Scale Stem Cell Bank Promotes Global Alzheimer's Disease Research
A groundbreaking large-scale stem cell bank has been developed to advance global research into the genetic factors influencing Alzheimer's disease, offering new hope for personalized treatments.
Gut Microbes and Acetate Synergy Promote Fat Loss in Mice Without Muscle Wastage
A recent study reveals that enhancing acetate levels in the gut, alongside specific Bacteroides bacteria, can reduce fat in mice without muscle loss, offering promising insights for obesity treatment through microbiome modulation.
Innovative Stem Cell Technique Accelerates Creation of Microglia for Brain Research and Disease Modeling
Harvard researchers have developed a swift and efficient method to generate human microglia-like cells from stem cells, enabling advanced neurodegenerative disease research and therapeutic development.
FDA Approves Pembrolizumab for Resectable Head and Neck Cancer with PD-L1 Expression
The FDA has approved pembrolizumab for treating resectable head and neck squamous cell carcinoma with PD-L1 expression, marking a major advancement in cancer immunotherapy based on promising clinical trial results.