Advances in Nervous System Interfaces for Rehabilitation

Explore the latest advancements in neural interfaces and neuroprosthetics that are revolutionizing rehabilitation for neurological conditions through innovative stimulation, prosthetics, and bioengineering solutions.
Memory loss, tremors, and paralysis occur when parts of the nervous system deteriorate or are damaged, leading to severe health challenges. Addressing these issues involves exploring innovative methods to repair and restore neuronal functions. Scientists are developing various strategies to interface with the nervous system, aiming to reconnect or replace damaged pathways.
The human nervous system contains approximately 86 billion neurons, which peak before birth and gradually decline with age. While some neurogenesis occurs in specific brain regions, the body's innate ability to regenerate neurons or repair neural injuries is limited, especially compared to regenerative species like salamanders, which can regrow lost limbs. This limitation necessitates alternative approaches to healing neural damage.
Neuroplasticity—the brain's capacity to rewire and establish new connections—plays a vital role in rehabilitation. When neurons die or become non-functional, the remaining neural networks can adapt by forming new pathways, provided the damage isn't too extensive. Researchers at EPFL are working on methods to restore neural communication through stimulation, whether in the brain, spinal cord, or peripheral nerves. These approaches hold promise for translating into clinical therapies that can significantly improve patients' quality of life.
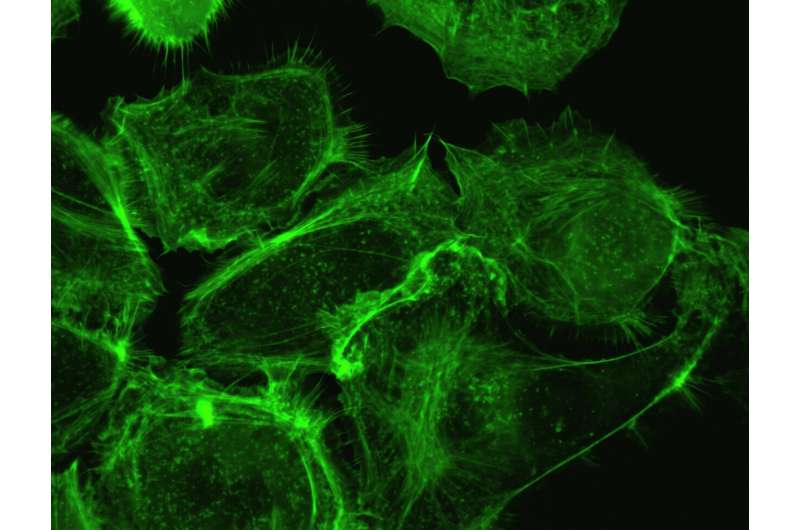
Prosthetic devices, both invasive and non-invasive, are at the forefront of neurorehabilitation. Implantable electrodes can directly interface with neural tissue, delivering electrical signals to stimulate or record activity. Non-invasive solutions rely on surface electrodes placed on the skin, while pharmaceutical methods aim to promote neuroplasticity and nerve regeneration using drugs and gene therapies.
Innovative developments include iontronics—systems that control ionic movement instead of electrons—offering a new language for communicating with neurons. Stretchable and biocompatible electrodes further enhance interface fidelity, conforming seamlessly to neural tissue to improve signal transmission.
Deep brain stimulation and spinal cord stimulation are also key techniques, with recent breakthroughs including FDA-approved spinal cord stimulation therapy for rehabilitation post-injury. Researchers are also exploring the use of deep brain stimulation to improve motor functions in conditions like Parkinson's disease.
Overall, the integration of neuroengineering, materials science, and biomedical research is paving the way toward sophisticated neural interfaces. These advancements aim to restore lost functions, improve recovery outcomes, and open new horizons for treating neurological disorders.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Research Finds Young Adults Do Not Adjust Consumption When Using High-Potency Cannabis
A new study finds young adults in the US do not adjust their cannabis consumption based on potency, leading to increased use and higher risk of disorder. Learn more about the implications of high-potency cannabis use.
Innovative Fall Prevention Program Supports Older Adults with Mild Cognitive Impairment
A groundbreaking fall prevention program utilizing passive monitoring and personalized coaching shows promise in reducing fall risks among older adults with mild cognitive impairment, enhancing safety and quality of life.
Stricter Gun Laws Linked to Fewer In-Home Pediatric Firearm Homicides
Research shows that stricter gun control laws at the state level are associated with a decrease in in-home firearm homicides among children and teenagers. Strong laws like red flag laws help protect vulnerable youth from firearm-related violence.