Persistent Use of Unnecessary Cancer Screenings Despite Updated Guidelines, New Study Reveals

A new study reveals that unnecessary cancer screenings persist for years after guidelines advise against them, leading to overdiagnosis and increased healthcare costs. The research emphasizes the need for better implementation of evidence-based practices.
A recent study highlights that unnecessary and potentially harmful cancer screenings continue for years even after official guidelines advise against them. Published in BMJ Quality & Safety, the research examines the lag between the dissemination of updated screening recommendations and their actual adoption in clinical practice, which can take up to 13 years or longer. This delay allows many patients to be subjected to overdiagnosis, unnecessary treatments, pain, anxiety, and increased healthcare costs.
The study emphasizes that for certain cancers, such as cervical and prostate cancer, the reduction in screening rates has been slow despite clear guidelines. For example, screening for cervical cancer in women under 21 or over 65 dropped by 50% within a year, but in women over 65, it took over a decade to reach similar reductions. Similarly, although guidelines have recommended against prostate cancer screening in men aged 70 and above since 2012, screening rates have not decreased sufficiently.
Barriers to stopping unnecessary screenings include ingrained medical routines, patient expectations, and the challenge physicians face when changing long-standing practices. The lack of mechanisms to accurately track the impact of updated guidelines on screening behaviors for cancers like ovarian, thyroid, testicular, and pancreatic further complicates the issue.
Guidelines for cancer screenings are established by the U.S. Preventive Services Task Force, which grades the appropriateness of tests based on evidence, with 'D' grades indicating tests that should generally not be performed due to lack of benefit or potential harm. Despite periodic updates, the persistence of outdated screening practices underscores the need for better implementation strategies and education to reduce low-value procedures.
Ultimately, the study advocates for increased efforts to align clinical practice with current evidence-based guidelines, to minimize patient harm, optimize resource use, and improve healthcare outcomes.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Implantable Cardioverter Defibrillators Show No Mortality Benefit in Certain Heart Attack Patients
New research at ESC 2025 suggests that implantable cardioverter defibrillators may not reduce mortality in certain post-heart attack patients with moderate LV dysfunction and arrhythmia risk markers.
The Importance of Sexual Orientation and Gender Data in Public Health
Understanding and collecting data on sexual orientation and gender identity are essential for addressing health disparities and effectively managing public health crises within LGBTQ+ communities. Recent policy restrictions threaten to undermine these efforts, risking overlooked health issues and wider societal impacts.
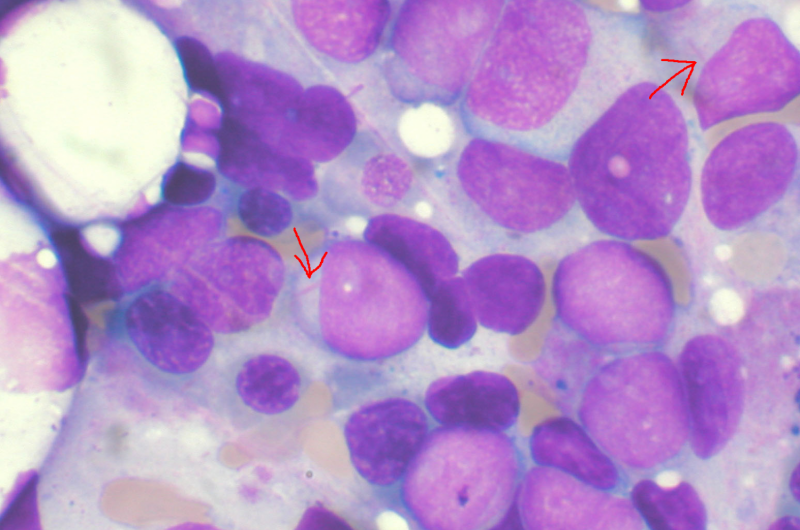
New Surface Protein Mechanism Identified in Leukemia Cells to Evade Immune System
Lund University researchers have identified a surface protein, SLAMF6, that helps leukemia cells evade immune detection. Blocking this protein may lead to new targeted therapies for resistant AML.
Diverse Genetic Origins of Autism May Result in Common Brain Function and Behaviors
New research suggests that different genetic variants of autism can result in similar brain activity patterns and behaviors, offering insights into shared neural mechanisms across diverse forms of autism.