Understanding Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Beyond Fatigue

Myalgic Encephalomyelitis/Chronic Fatigue Syndrome is a complex neurological disorder affecting multiple body systems, characterized by persistent fatigue, post-exertional malaise, and cognitive difficulties. Learn about its symptoms, diagnosis challenges, and the latest scientific insights.
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a complex and often misunderstood neurological condition that extends far beyond the common perception of fatigue. Frequently labeled as simply 'chronic fatigue,' this illness involves a wide array of symptoms that significantly impact patients' lives. Recognized by the World Health Organization, ME/CFS affects nearly every system in the body, including the nervous, immune, vascular, and muscular systems.
The term reflects hallmark features such as muscle pain (myalgia), inflammation of the brain (encephalomyelitis), and profound, persistent fatigue that rest cannot alleviate. The illness predominantly impacts middle-aged adults and is two to three times more common in women. Though the exact cause remains unknown, a common trigger is often an infection.
Core symptoms include debilitating fatigue that lasts for at least six months, worsened by physical or mental exertion—a condition known as post-exertional malaise. Even minimal activity, like showering or social interactions, can trigger worsening symptoms that may persist for days. Other symptoms encompass sleep disturbances, cognitive impairments (such as memory and decision-making difficulties), pain, dizziness, gastrointestinal issues, heart rate irregularities, and flu-like sensations.
The severity varies: some individuals manage symptoms enough to continue working, while others become housebound or bedridden. The fluctuating nature of symptoms over time further complicates diagnosis and management.
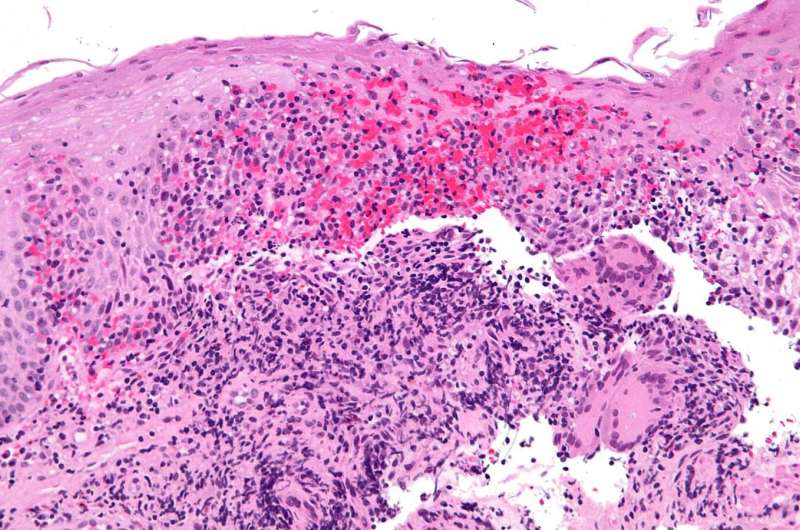
Scientific research increasingly confirms that ME/CFS is a biological disorder, with neuroimaging studies revealing differences in brain structure and activity, including reduced blood flow and neurotransmitter levels. Additional research points to alterations in energy production, immune function, oxygen delivery, and blood pressure regulation, underscoring its physiological basis.
Diagnosing ME/CFS involves excluding other causes of fatigue through clinical criteria, but inconsistent diagnostic standards worldwide pose challenges for research and treatment. Some criteria emphasize only fatigue, risking misdiagnosis, while others focus on more severe symptom presentations. This variability hampers the ability to compare studies and develop uniform treatment strategies.
Treatment guidelines vary according to different health authorities. In Australia, current practices rely on outdated criteria, emphasizing graded exercise therapy and cognitive behavioral therapy, despite evidence that physical activity can worsen symptoms. Recent updates advocate for updated, evidence-based approaches, recognizing the potential harm of pushing beyond one's energy limits.
Currently, managing ME/CFS focuses on symptom pacing—working within individual energy envelopes—and early rest during illness onset. Preserving energy and avoiding overexertion can lead to better long-term outcomes. The emergence of long COVID has heightened awareness of post-viral syndromes, with many affected individuals meeting ME/CFS criteria.
While waiting for updated clinical guidelines, patients are encouraged to listen to their bodies, prioritize rest, and avoid strenuous activity during flare-ups. Continuing research aims to refine diagnosis and treatment, with increased governmental support promising better understanding and care in the future.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Alcohol Consumption Linked to Increased Dementia Risk: New Research Finds No Safe Level
New large-scale research indicates that any level of alcohol consumption may increase the risk of dementia, with no evidence supporting protective effects of moderate drinking. Reducing alcohol intake is advised for brain health.
Potential of Alzheimer's Medication to Improve Social Skills in Youth with Autism
A groundbreaking study suggests that memantine, an Alzheimer's drug, may enhance social skills in youth with autism, especially those with elevated brain glutamate levels, paving the way for personalized treatments.
Innovative Mini-Lungs with Blood Vessels Developed, Advancing Pulmonary Disease Research
Researchers at UCLA have developed vascularized mini-lungs from stem cells, offering new insights into lung development and pulmonary vascular diseases, with potential for drug testing and personalized treatments.
promising new investigational treatment shows potential for Crohn's disease remission
A new investigational therapy targeting TL1A shows significant potential to induce remission in Crohn's disease, offering hope for better treatment options. Recent studies highlight rapid response and possible effects on fibrosis crucial in disease management.