Long-Term Care Residents Face Severe Disability and Loss of Independence: A Growing Concern

Recent research highlights a troubling trend among residents of long-term care (LTC) facilities: a significant proportion experience severe, often lasting impairments that profoundly diminish their quality of life. Within five years of admission, approximately 20% of residents become permanently unable to make daily decisions for themselves, such as choosing their meals or clothing. Many of these individuals live with severe cognitive and physical disabilities, sometimes for over two years, leading to a state where communication and personal independence are severely compromised.
The study, conducted by the Bruyère Health Research Institute and ICES, analyzed data from over 120,000 adults aged 65 and older admitted to LTC facilities in Ontario between 2013 and 2018. Researchers found that around 13% of residents transitioned to complete dependence for all personal care, including bathing, toileting, and eating, often for more than 45 days. Notably, younger seniors under 80 and those with dementia tended to live longer after reaching this level of dependence.
A critical aspect of the findings relates to residents' end-of-life preferences. The study observed that individuals with do-not-resuscitate (DNR) or do-not-hospitalize orders often experienced a shorter duration of severe disability, indicating that advance care planning plays a vital role in aligning care with personal values. According to lead author Ramtin Hakimjavadi, residents frequently report that losing independence is more distressing than dying itself. Therefore, healthcare providers should foster open discussions about quality of life, potential disabilities, and end-of-life wishes.
The data also revealed that 65% of residents had a DNR order, and 25% had do-not-hospitalize directives, which likely contributed to better alignment of care with their preferences. Experts emphasize the importance of planning ahead to support dignity and comfort during the final stages of life, encouraging residents and their families to consider personal values when making care decisions.
This research underscores the need for comprehensive, resident-centered care approaches that address not only physical health but also the psychological and emotional impacts of severe disability. As more individuals enter long-term care, understanding and planning for these possible outcomes are essential for ensuring respectful and dignified end-of-life experiences.
Source: https://medicalxpress.com/news/2025-04-severe-impairment-worse-death-affects.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
Can Reducing Caffeine Intake Enhance Dream Vividness? Scientific Insights
Reducing caffeine intake can improve sleep quality and increase REM sleep, potentially leading to more vivid and memorable dreams. Discover the science behind caffeine's impact on dreaming.
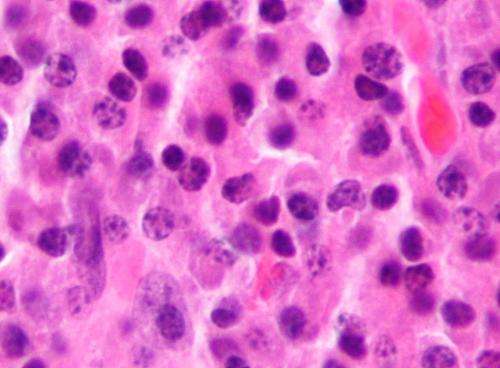
Nearly Doubling of Survival Rates in Myeloma Patients Since 2005
New research shows that survival rates for myeloma patients in the UK have nearly doubled since 2005, driven by new treatments and clinical trial participation, offering hope for improved outcomes in blood cancer care.
Osteoporosis Treatment Benefits for Individuals Over 80 Years Old
New research suggests that osteoporosis treatment for individuals over 80 who suffer fractures can significantly reduce hospitalization and mortality, emphasizing the importance of personalized care in aging populations.
Advanced AI Technology Enhances Lung Cancer Detection Through Exosome Stiffness Analysis
Scientists have developed an AI-powered method to detect lung cancer early by analyzing the stiffness of exosomes, enabling precise, non-invasive diagnosis through advanced nanomechanical techniques.