Innovative Antibody-RNA Treatment Shows Promise Against Resistant Tumors

A novel antibody-RNA therapy developed by Yale University researchers shows promising results in targeting resistant tumors like pancreatic, brain, and skin cancers, paving the way for personalized cancer treatments.
A groundbreaking study has introduced a specially engineered antibody capable of delivering RNA-based therapies directly into difficult-to-treat and resistant tumors. This novel approach, tested in animal models, has demonstrated significant improvements in survival rates and reductions in tumor sizes across various cancer types, including pancreatic, brain, and skin cancers. The antibody, named TMAB3, combined with immune-stimulating RNA, targets cancer cells with high precision, navigating through biological barriers like the blood-brain barrier to reach tumor sites.
Researchers from Yale University, led by senior author Peter Glazer, developed this technology by modifying the antibody to bind RNA and 'humanizing' it to prevent immune rejection. Computer modeling further enhanced its ability to target cancer cells specifically. The approach was tested in models of pancreatic ductal adenocarcinoma, medulloblastoma, and melanoma, all typically resistant to conventional therapies.
Results revealed that in pancreatic cancer models, the treatment significantly shrank tumors and increased survival by boosting CD8+ T cell activity. In brain tumor models, the therapy effectively bypassed the blood-brain barrier to reach and reduce tumor growth without causing collateral immune reactions. Melanoma models showed a notable suppression of tumor growth with minimal side effects.
This research offers a new pathway to deliver RNA therapies precisely to tumors, minimizing systemic toxicity and tailoring treatment to individual immunological contexts. The scientists also worked to humanize and optimize the antibody for potential clinical applications, aiming to move this platform into human trials. The findings suggest a promising future for personalized immuno-RNA therapies, particularly for 'cold' tumors that are resistant to current treatments.
Source: Science Translational Medicine
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
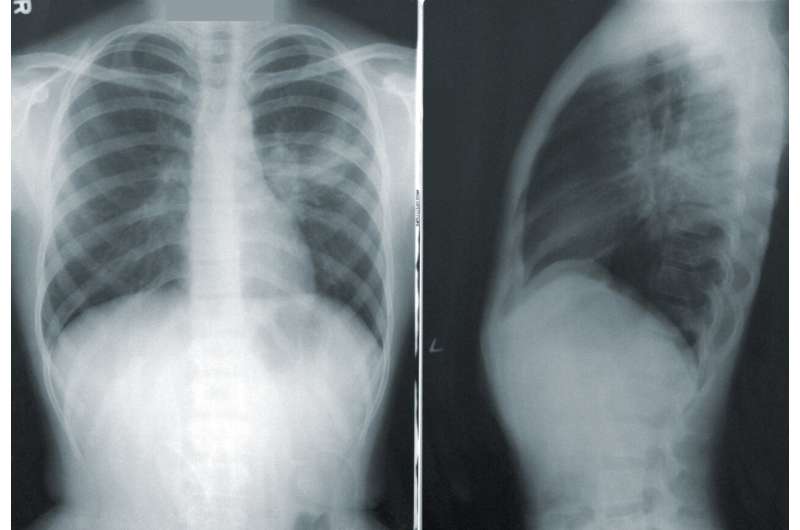
Rising Lung Cancer Rates Among Nonsmokers and the Underlying Causes
Increasing lung cancer cases among nonsmokers highlight the importance of awareness, early detection, and understanding environmental and genetic risk factors. Learn more about this evolving health issue.
Innovative AI Method Measures and Monitors Aging Cells
A cutting-edge AI-powered technique for measuring and tracking cellular senescence offers new insights into aging and age-related diseases, paving the way for potential therapies.
Genetic Factors Influencing Cardiomyopathy Risk in Childhood Cancer Survivors Vary by Age of Onset
New study identifies how genetic variants influence the risk of late-onset cardiomyopathy in childhood cancer survivors, highlighting differences from adult survivors and the general population.
New Therapeutic Target Identified to Prevent Breast Cancer Relapse by Eliminating Dormant Cells
Canadian scientists have identified PIK3C3 as a key protein for dormant breast cancer cell survival, paving the way for therapies to prevent metastasis and relapse. This breakthrough offers new hope for reducing recurrence and improving long-term outcomes for breast cancer patients.