Genetic Insights Reveal Variability in Insulin Loss Speed in Type 1 Diabetes Patients

New genetic research identifies factors influencing the speed of insulin depletion in type 1 diabetes, paving the way for personalized treatment approaches and improved disease management.
Recent research from Japan has shed light on the genetic factors influencing the rapid or slow progression of insulin depletion in individuals with type 1 diabetes (T1D). The study, involving a cohort of 314 Japanese patients, utilized detailed longitudinal data over up to 14 years to identify key genetic markers and clinical predictors that determine how quickly patients lose pancreatic insulin-producing β-cell function.
T1D is an autoimmune disease characterized by the immune system attacking insulin-producing cells, but the rate at which this occurs can differ significantly among patients. The Japanese study, published in the journal Diabetes Care, focused on the role of human leukocyte antigen (HLA) genes, which are known to affect both susceptibility and disease progression.
Participants were classified into three subtypes: acute-onset, slowly progressive (SP), and fulminant. The findings revealed that five years post-diagnosis, a substantial proportion of fulminant patients (93%) had no detectable insulin secretion, compared to only 9% of SP patients and 43% of acute-onset cases. Yet, within each subtype, there was notable variability in disease progression.
Genetic analysis highlighted that individuals with the DR4/DR4 genotype, particularly the DRB104:05-DQB104:01 haplotype, tended to retain β-cell function longer, earning them the label of "slow progressors." Conversely, heterozygous carriers of other HLA combinations, such as DR4/DR8 and DR4/DR9, experienced faster loss of insulin secretion, categorized as "rapid progressors."
Professor Shinsuke Noso emphasized that these genetic patterns influence not only disease risk but also its trajectory, paving the way for more personalized treatment strategies. Additionally, clinical factors such as low body mass index, presence of glutamic acid decarboxylase autoantibodies, and absence of protective haplotypes were linked to quicker disease progression in specific subtypes.
The implications of these findings are significant for clinical practice. Knowing a patient’s HLA genotype could help healthcare providers estimate the pace of β-cell decline and tailor interventions accordingly. Early use of advanced insulin delivery systems or immunotherapies like anti-CD3 antibodies could be timed more precisely to preserve pancreatic function.
This study marks a milestone in Japan's efforts to understand T1D through the TIDE-J cohort, a nationwide, multicenter initiative launched in 2010. It underscores the importance of combining genetic insights with clinical data to enhance personalized care, potentially delaying disease onset and preserving insulin production in some patients.
Funding and collaboration from multiple Japanese health and diabetes research institutions, including the National Center for Global Health and Medicine, underpin this pioneering research. As such, these insights hold promise not only for improving individual outcomes but also for transforming standards of diabetes care in Japan and globally.
Source: https://medicalxpress.com/news/2025-06-genetic-clues-insulin-depletion-patients.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
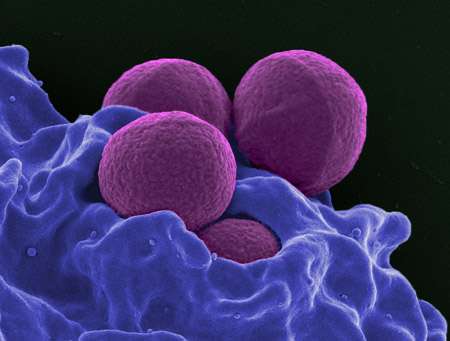
WHO Calls for Accelerated Action Against Drug-Resistant Superbugs
The WHO warns that the global pipeline for new antibiotics and diagnostics is dangerously limited, risking a surge in drug-resistant infections worldwide. Urgent investment and innovation are needed to combat antimicrobial resistance effectively.
Innovative Vibration-Driven Chip Promises to Transform Fertility Treatments
A pioneering vibration-driven chip developed at Cornell University could revolutionize assisted reproductive technology by streamlining oocyte cumulus removal, making fertility treatments more accessible and efficient worldwide.
Innovative Approach Using Stem Cells and Drug Therapy to Combat Abnormal Bone Growth in FOP
A novel therapy combining stem cells and rapamycin effectively reduces abnormal bone formation in FOP, a rare genetic disorder, improving mobility and offering hope for future treatments.
Debunking Concerns About Calcium Supplements and Dementia Risk
New research shows that calcium supplements do not increase dementia risk in older women, reassuring clinicians and patients about their safety for brain health.