Emergency Departments Implement Geriatric-Friendly Care to Better Serve Older Adults

Emergency rooms are evolving to meet the unique needs of the aging population, recognizing that older patients face specific challenges in the high-stimulation environment of an emergency department (ED). The typical ER environment—with bright lights, loud noise, and crowded spaces—can be disorienting, increase fall risks on slick floors, and trigger acute confusion or delirium, especially in older individuals.
To improve care for seniors, many hospitals are adopting geriatric or age-friendly ED models. Historically, emergency teams treated all patients the same, but now there's a shift toward tailored approaches that acknowledge the distinct medical and psychosocial needs of older adults. This change has gained momentum worldwide; in the U.S. alone, over 500 hospitals have achieved accreditation for geriatric emergency care through the American College of Emergency Physicians, reflecting a rapid expansion of such initiatives.
Geriatric-friendly EDs focus on physical modifications and protocol adjustments to enhance patient safety and comfort. Physical adaptations include non-slip flooring, abundant handrails, assistive devices like walkers, clear signage, and large-print documentation to accommodate visual impairments. Protocols emphasize the evaluation of cognitive status, medication review, mobility, and what is termed the '4Ms' framework—what matters most to patients, medications, mental status, and mobility—ensuring comprehensive, patient-centered care.
Assessment begins with screening for cognitive impairments such as dementia, which can influence treatment decisions and response to care. Many symptoms presented—like dizziness or falls—may stem from underlying issues such as stroke or medication effects, warranting thorough investigation. Furthermore, older adults often are on multiple complex medications, which require careful review since organ function declines with age, potentially altering drug metabolism and dosing.
Understanding each patient's goals is crucial. While younger patients may seek full diagnostics and hospital stays, older adults often prioritize symptom relief and management of chronic conditions. Some may opt for comfort or hospice care over aggressive treatment. Age-friendly ICUs also help prevent complications like delirium, which is linked to worse outcomes, through hydration, minimized equipment use, and creating calmer environments.
The benefits of geriatric emergency care are significant. Patients report higher satisfaction levels, and such approaches can reduce unnecessary hospital admissions, lowering healthcare costs. For example, studies show that targeted interventions in the ED can decrease re-admissions and falls, ultimately improving health outcomes.
Despite the growth, only a small proportion of EDs are fully certified as geriatric-friendly, with rural hospitals increasingly pursuing accreditation to serve their aging communities better. While emergency care is often dictated by immediate needs—such as stroke or heart attack treatment—patients with less urgent concerns still benefit from age-sensitive protocols that ensure safety and dignity.
Looking ahead, expanding and standardizing geriatric emergency protocols across healthcare systems remains a priority, aiming to provide respectful, effective, and safe care for older adults everywhere.
Source: https://medicalxpress.com/news/2025-05-emergency-rooms-older-adults.html
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
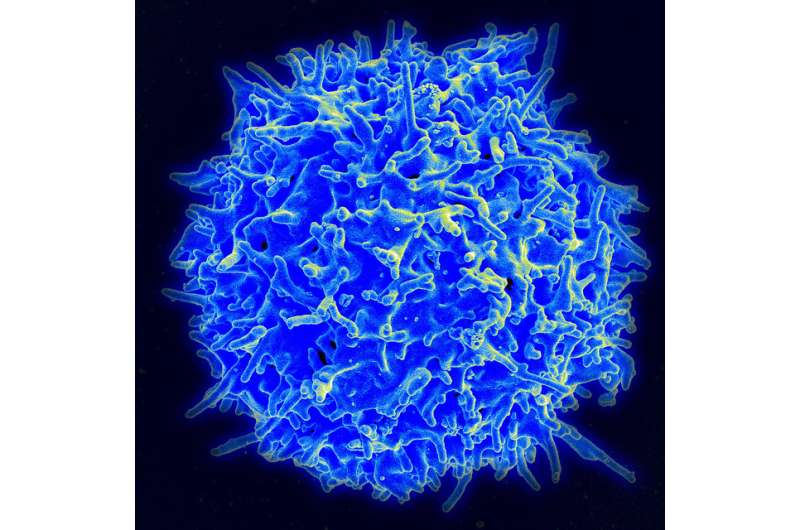
Innovative Engineered Antibodies Enable T-Cells to Target and Destroy Cytomegalovirus-Infected Cells
Researchers have engineered bispecific antibodies that direct T-cells to effectively target and eliminate cytomegalovirus-infected cells, offering new hope for immunocompromised patients battling CMV infections.
The Future of Immunization: Innovations in Nasal Vaccines
Nasal vaccines offer a promising, needle-free approach to boost immunity against respiratory viruses, with potential to reduce disease severity and transmission. Discover the latest advancements and challenges in this innovative field.
Addressing Gaps in Substance Use Disorder Treatment: New Community-Driven Approaches
Researchers from Michigan State University have developed data-driven tools to improve substance use disorder treatment and address regional disparities in Michigan, with a focus on community-specific needs and policy impact.
Enhancing Road Safety Through Shared Responsibility and Innovation
A comprehensive approach involving shared responsibility and technological innovation is vital to reducing roadway fatalities and creating safer transportation systems for all road users.