The Vital Impact of Community and Family Support on Health Behavior Change and Outcomes

Research highlights the critical role of community and family support in changing health behaviors and reducing cardiovascular disease risk among Latino populations through culturally tailored interventions and systemic improvements.
A recent qualitative study conducted by researchers from the UC Irvine Joe C. Wen School of Population & Public Health sheds light on the crucial influence of community and family involvement in promoting heart-healthy behaviors among Latino families in Orange County, California. This study provides valuable insights into how cultural understanding, social support networks, and systemic challenges affect cardiovascular health management.
The research highlights that many community members have limited knowledge about cardiovascular disease (CVD), including symptoms, risk factors, and preventive strategies. Cultural norms such as gender roles and stigmas influence health attitudes and behaviors, particularly among men, who may be less likely to seek care or adopt lifestyle changes. Barriers such as transportation issues, work schedules, and limited access to technology further hinder engagement in health-promoting activities.
Conversely, family support and community health workers (CHWs) play a pivotal role in facilitating behavior change. Support from relatives in tasks like meal preparation, blood pressure monitoring, and technology use significantly reinforces healthy routines. The study identified that culturally tailored interventions—such as cooking classes, meal planning across generations, and community events—enhance engagement and foster sustainable habits.
At the community level, structural hurdles like food insecurity, neighborhood safety concerns, and limited access to preventive health services pose significant challenges. Participants emphasized the need for affordable health education, safer public spaces, and partnerships with local organizations to create healthier environments.
Additionally, the research underscored the complex relationship between nutrition and CVD. Traditional cooking practices, food costs, and time constraints hinder the adoption of heart-healthy diets. In response, the intervention incorporated culturally relevant cooking programs and community activities that promote healthy eating.
Long-term behavior change relies heavily on intergenerational support networks. Relatives assist with practical tasks, believe in shared health goals, and help bridge health literacy gaps. However, barriers such as unsafe parks, fears related to immigration status, and homelessness limit health-promoting opportunities. The SERVE OC team works closely with community stakeholders to address these systemic issues, aiming to improve neighborhood safety, access to nutritious foods, and healthcare services.
This approach exemplifies how engaging communities directly in health interventions can produce more effective and equitable outcomes. By elevating community voices and addressing both behavioral and structural factors, programs like SERVE OC are paving the way for meaningful improvements in cardiovascular health among underserved populations.
Ultimately, the study demonstrates that culturally sensitive, family-centered strategies, combined with systemic reforms, are essential for reducing disparities and fostering lasting health improvements. Insights from this research can inform future public health initiatives that prioritize community engagement and equitable healthcare access.
Stay Updated with Mia's Feed
Get the latest health & wellness insights delivered straight to your inbox.
Related Articles
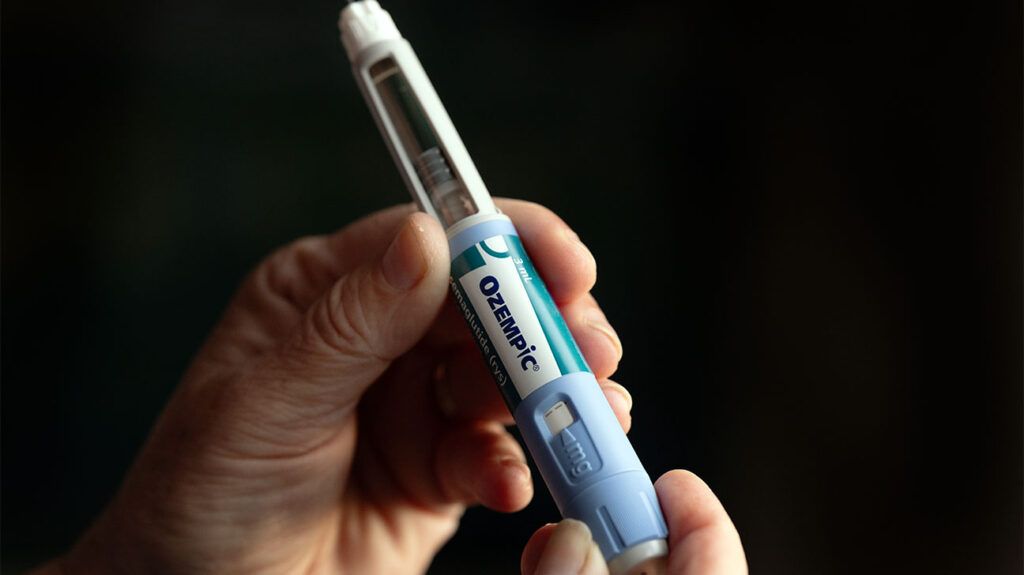
Semaglutide Shows Promise in Reducing Heart Disease Risk Within Six Months
Emerging research suggests that semaglutide, a diabetes and weight loss medication, may reduce the risk of major heart events within just six months of treatment, offering promising cardiovascular protection for at-risk individuals.
Rifampin Shows 99.9% Effectiveness Against Typhoid Fever
Discover how rifampin, a widely used antibiotic, is showing remarkable promise with 99.9% effectiveness against typhoid fever by removing bacterial protective capsules, offering new hope in fighting resistant strains.
Expansion of West Nile Virus Threat in San Diego County
West Nile virus activity is increasing in San Diego County, with recent detections in neighborhoods and ongoing mosquito control efforts, highlighting the need for preventative measures against mosquito bites.
Limitations of Current Biomarkers in Assessing Post-Pregnancy Heart Failure Risk
New research questions the effectiveness of traditional biomarkers like NT-proBNP for predicting heart failure in women after complicated pregnancies, emphasizing the need for new screening methods.